Nerve Block Gallery
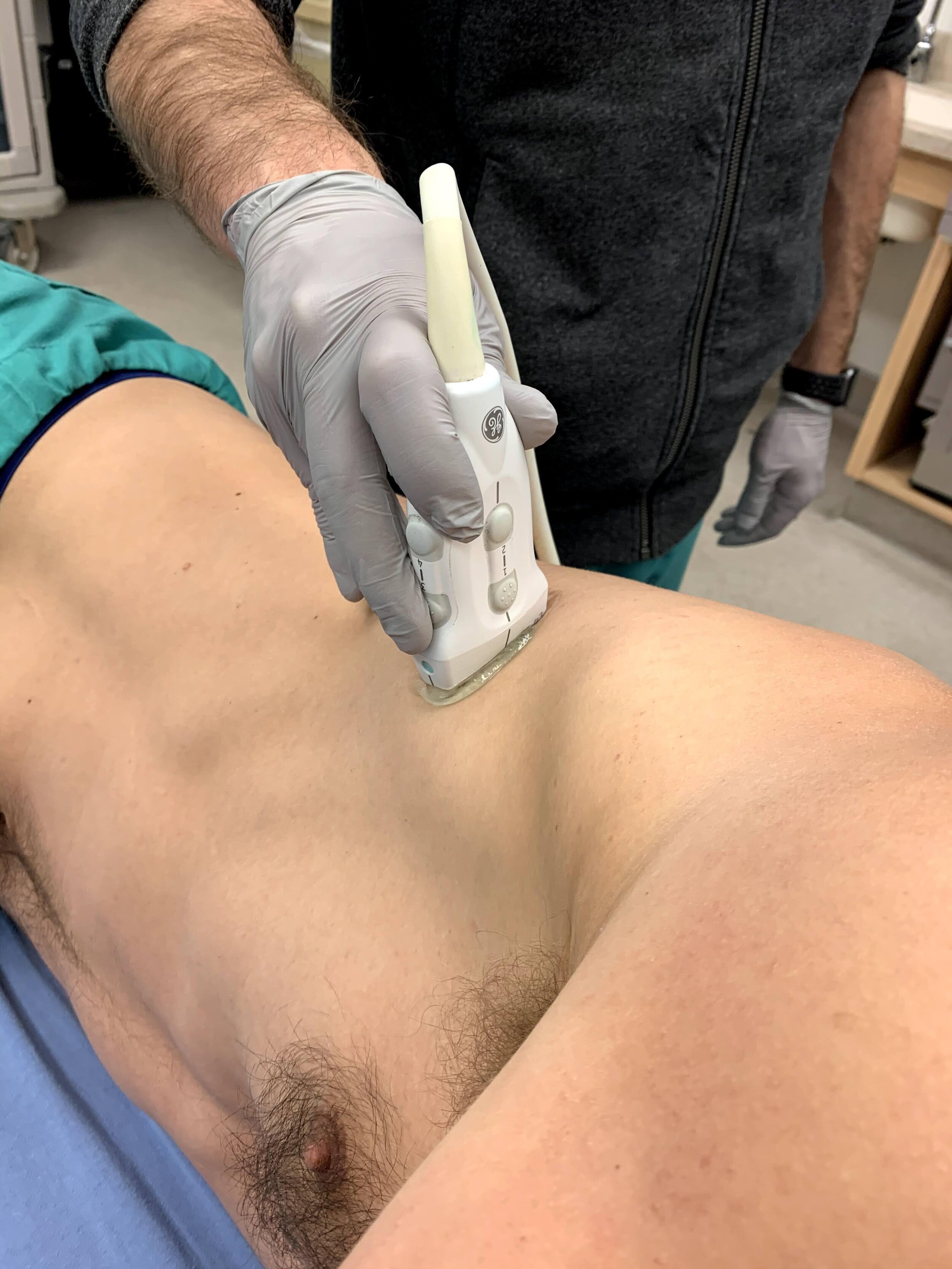
Left Popliteal Sciatic Nerve Block
20 year old female with a history of IV drug use presents with a sizable calf abscess. She is admitted to the hospital for sepsis criteria and abscess drainage.
She prefers no analgesia, therefore a popliteal sciatic nerve block is performed (demonstrated by injection of anesthetic adjacent to sciatic nerve) with resolution of her pain and successful incision and drainage.
Contributors: John Bowling, DO (@BModeBowling); Bob Stenberg, MD (@POCUSaurusRex)
Cleveland Clinic Akron General

Median Nerve Palmar Area of Anesthesia

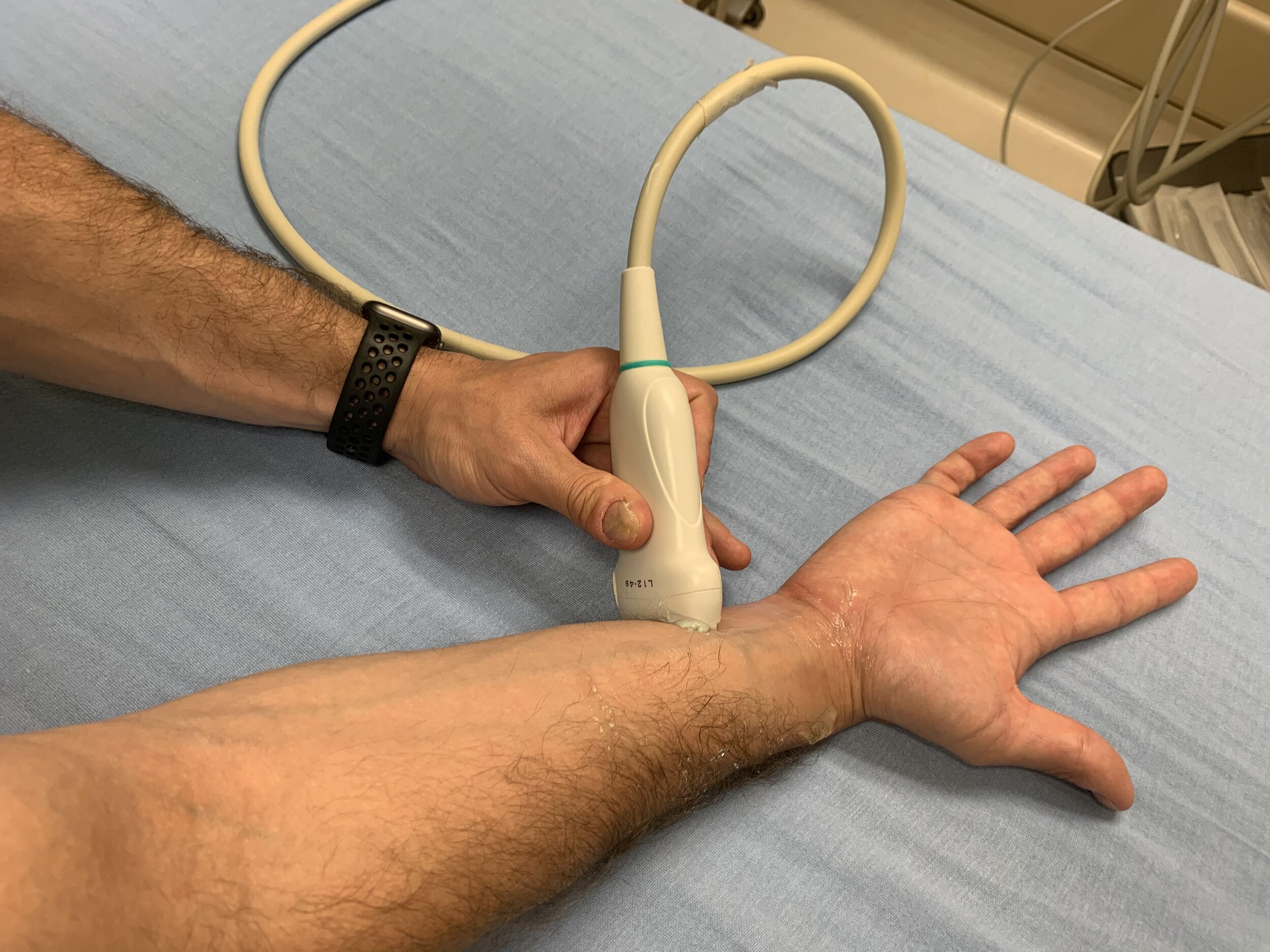
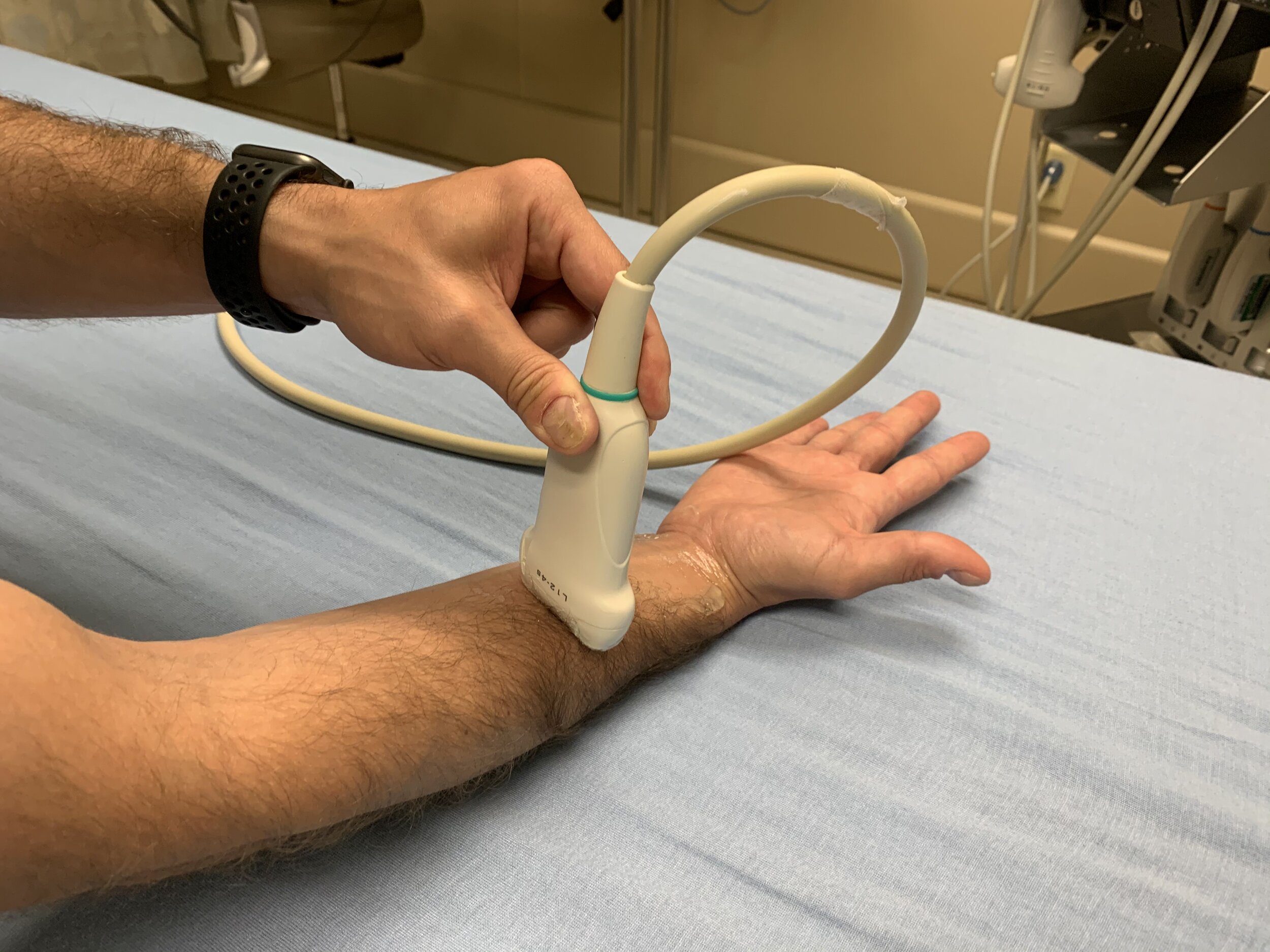
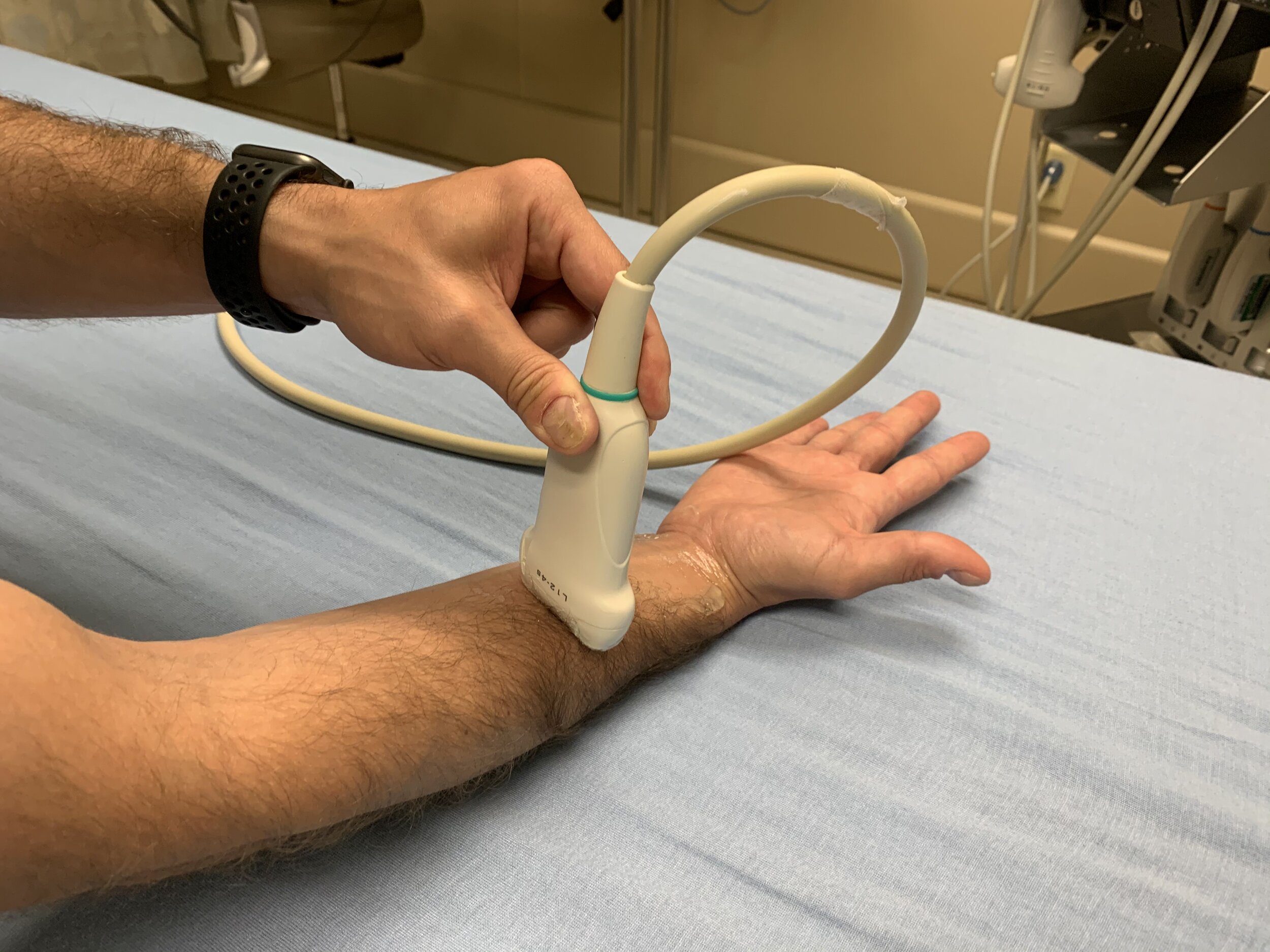
Median Nerve Probe Location
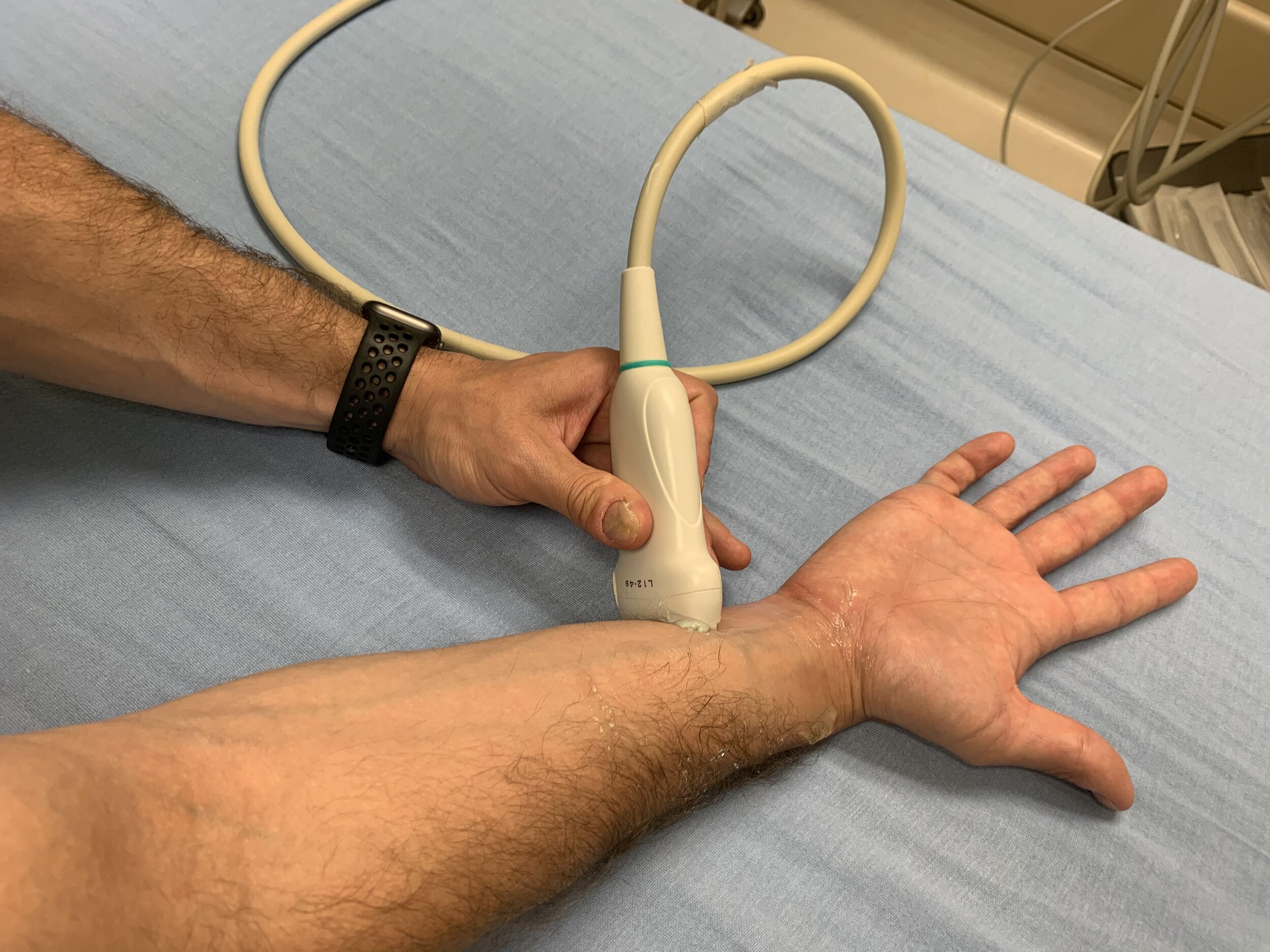
Ulnar Nerve Probe Location

Fascia Iliaca Area of Anesthesia

Fascia Iliaca Nerve Probe Placement
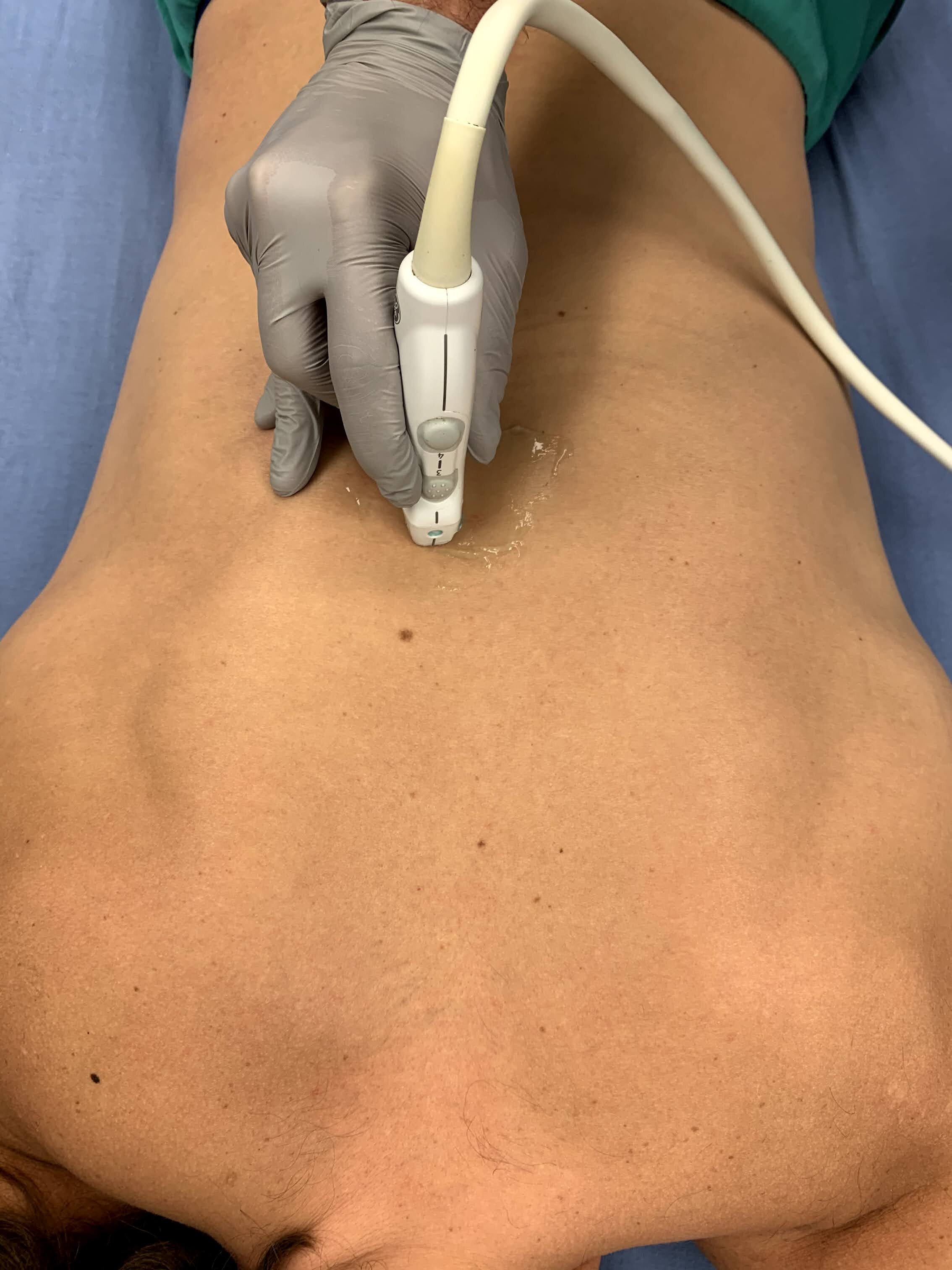
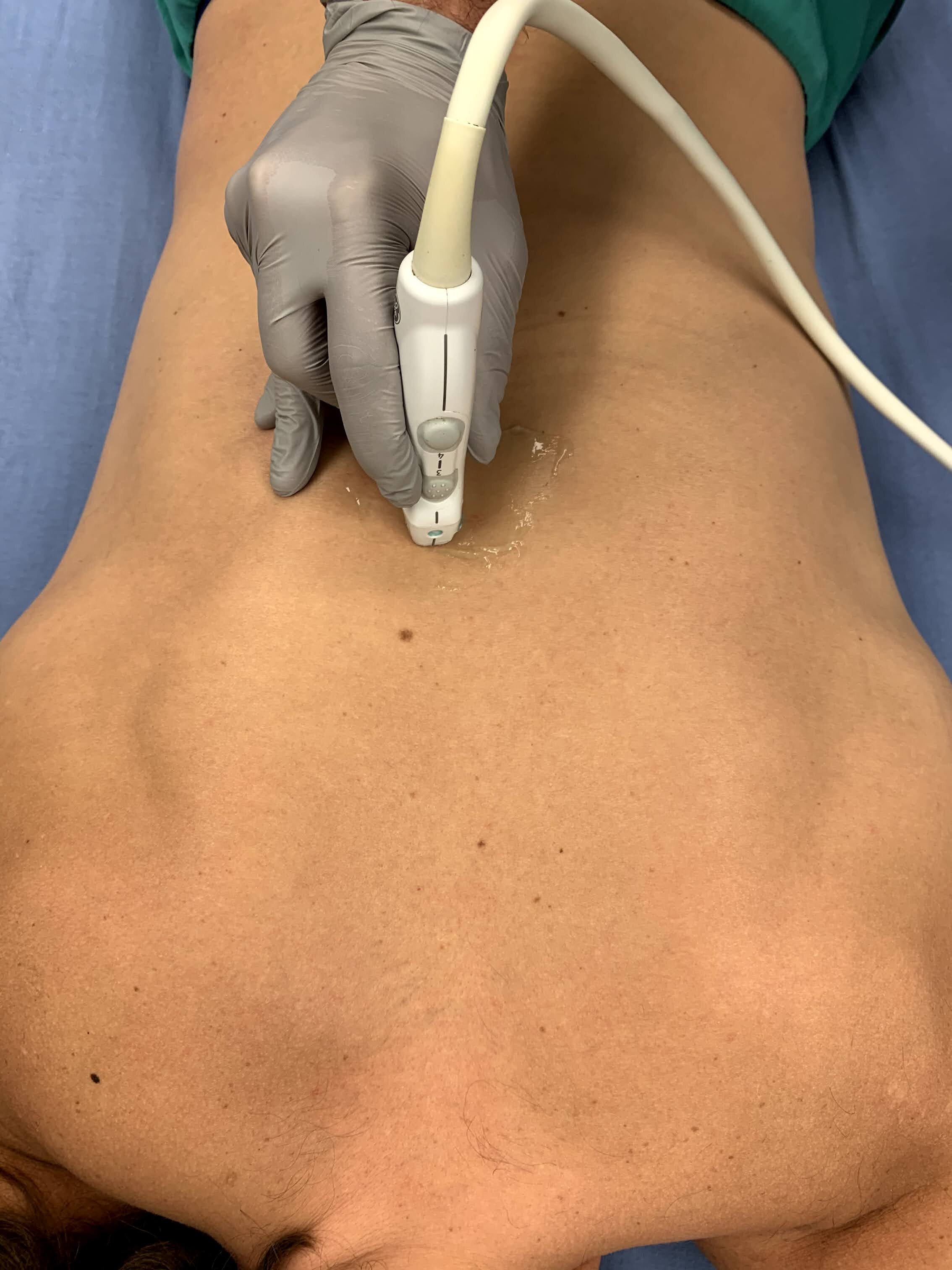
Erector Spinae Probe Location

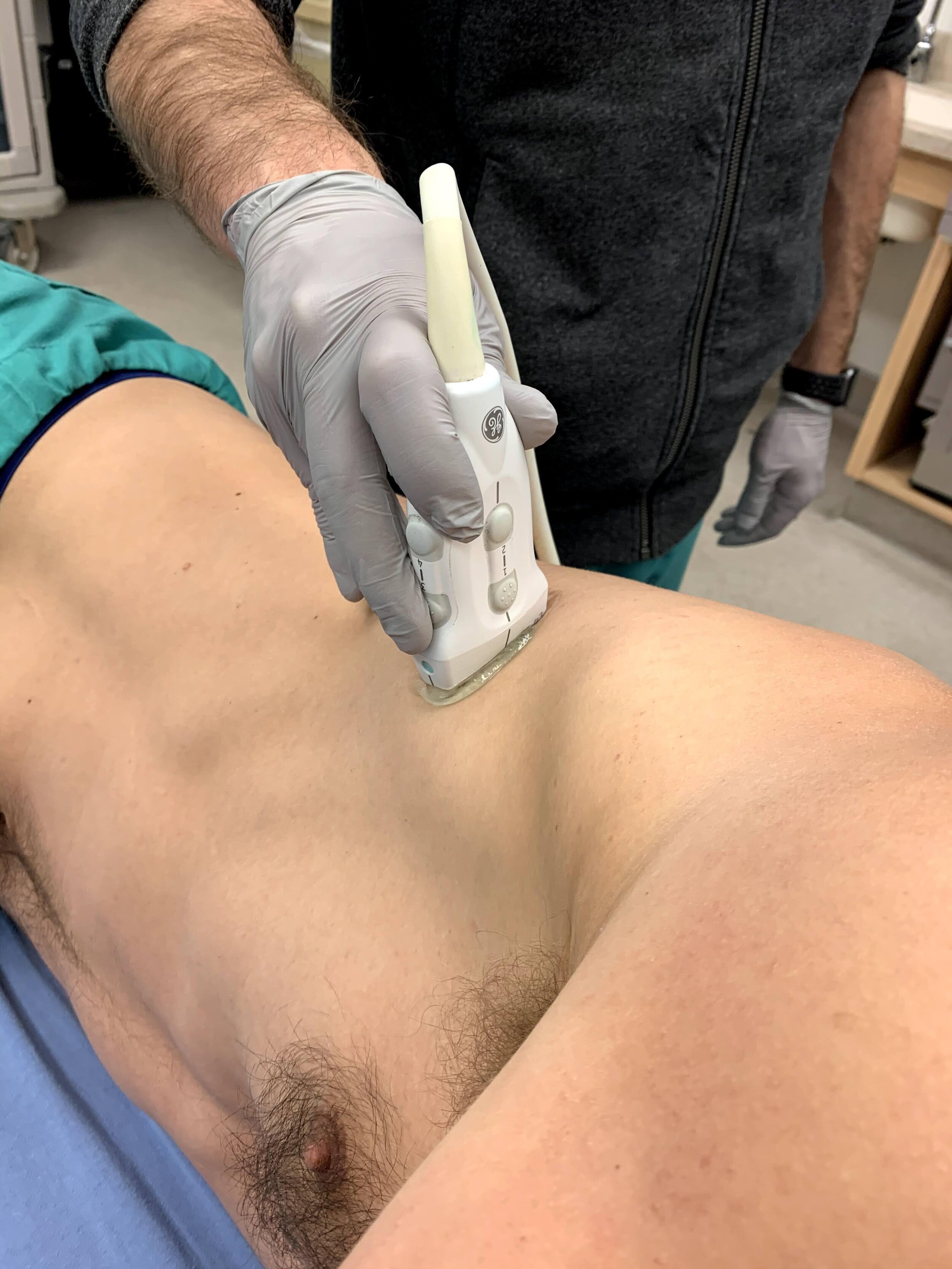
Infraclavicular Probe Placement

Interscalene Probe Placement

Popliteal Nerve Probe Location

Posterior Tibial Probe Location
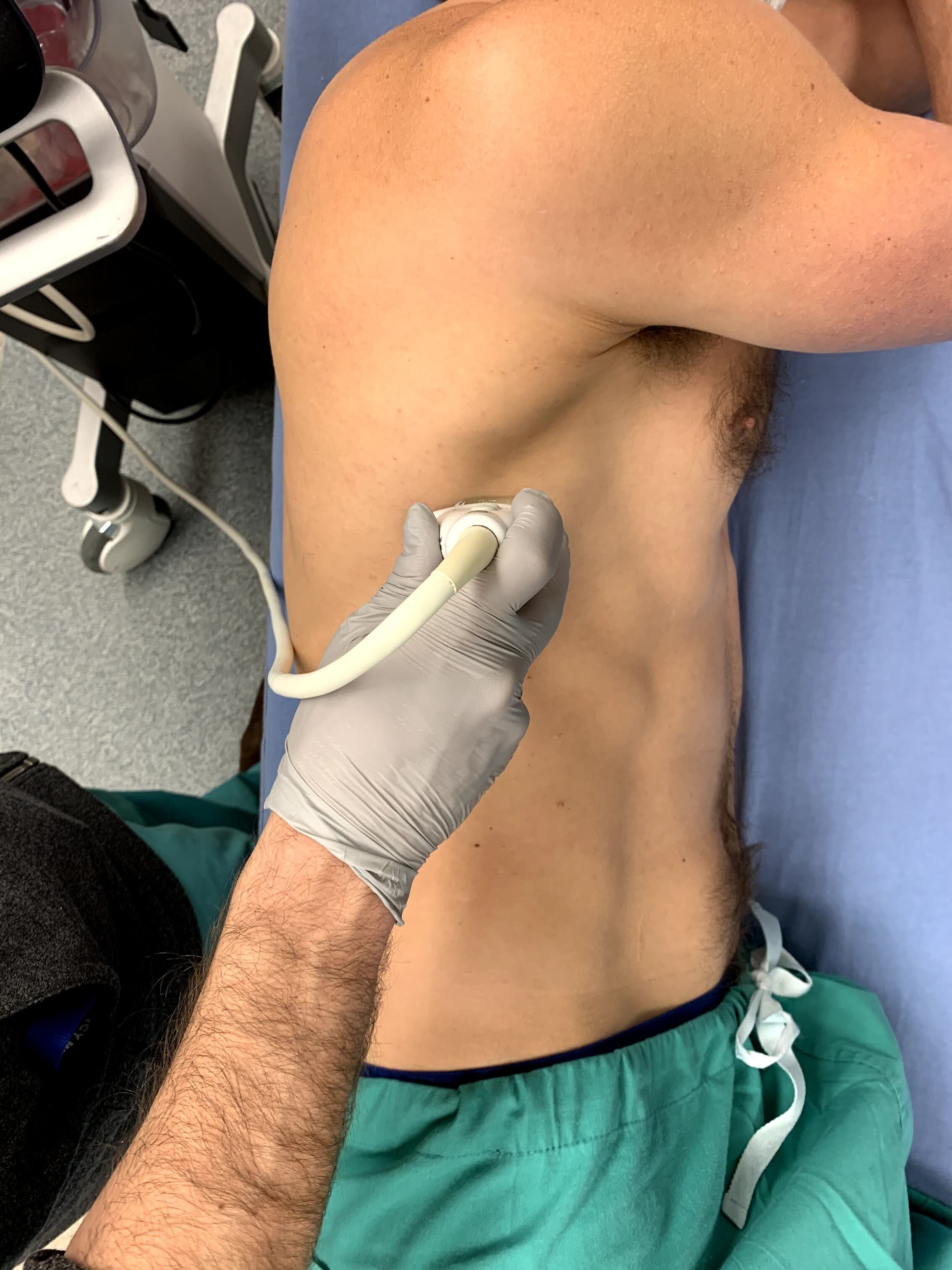
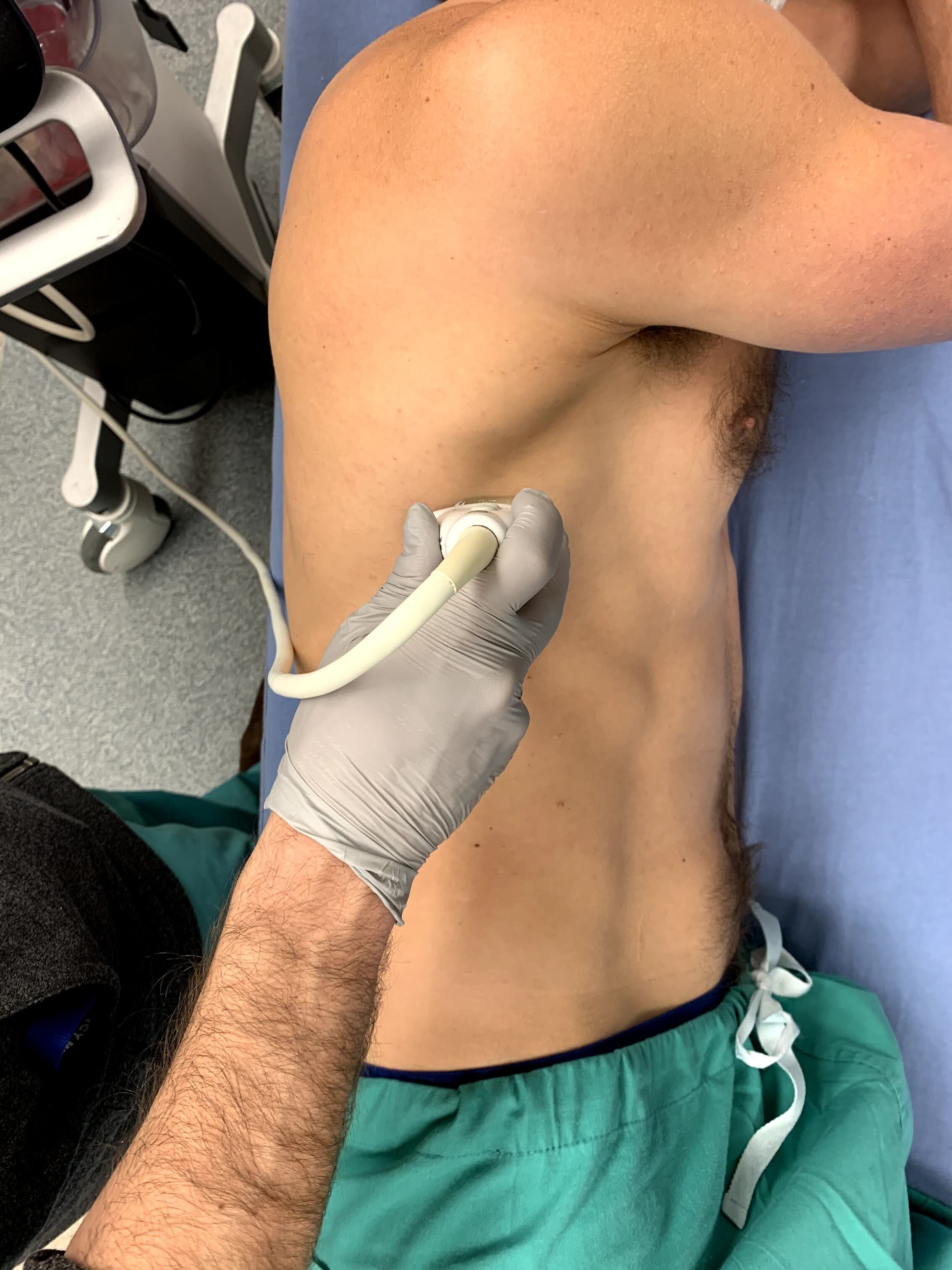
Serratus Anterior Probe Location
Serratus Anterior Probe Location
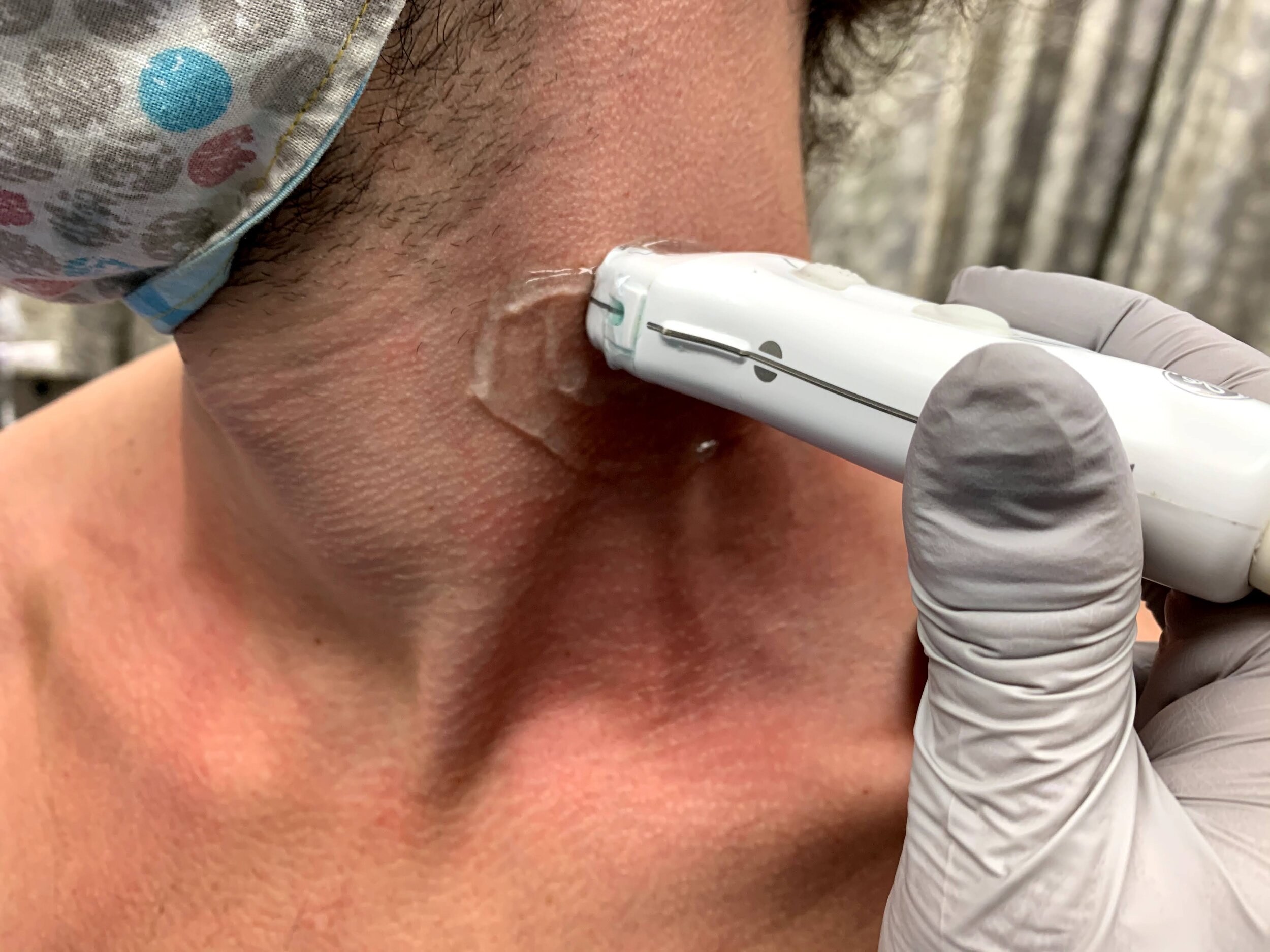
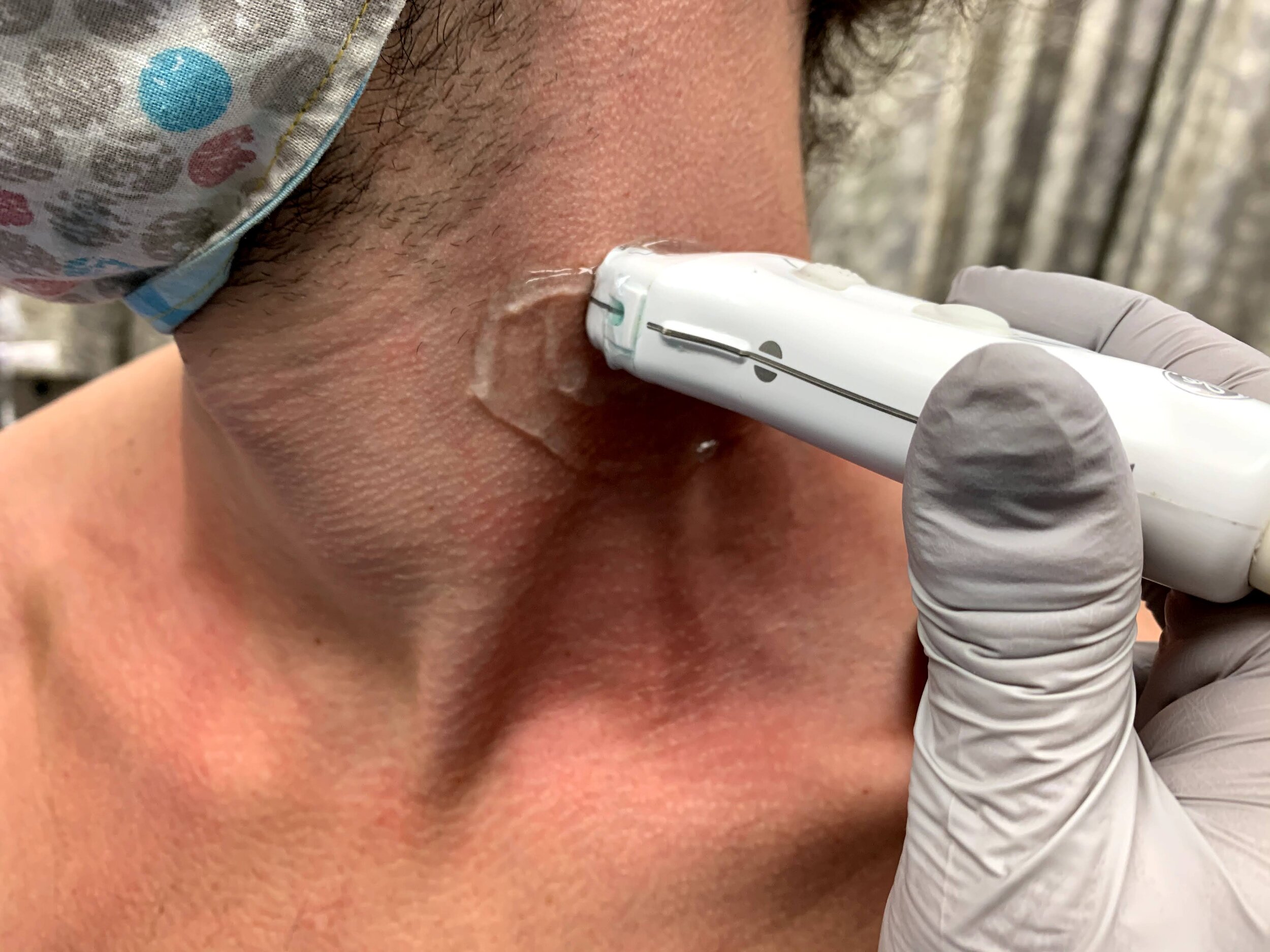
Superficial Cervical Probe Location

Supraclavicular Probe Location

Common Peroneal Nerve Area of Anesthesia

Popliteal Sciatic Nerve Area of Anesthesia

Posterior Tibial Area of Anesthesia

Radial Nerve Area of Anesthesia

Saphenous Nerve Area of Anesthesia

Saphenous Nerve Posterior Area of Anesthesia

Superficial Cervical Plexus Area of Anesthesia

Serratus Anterior Area of Anesthesia

Serratus Anterior Area of Anesthesia

Ulnar Nerve Area of Anesthesia

Ulnar Nerve Area of Anesthesia

Interscalene Area of Anesthesia

Interscalene Area of Anesthesia

Supraclavicular Area of Anesthesia

Supraclavicular Area of Anesthesia

Axillary Nerve Area of Anesthesia

Axillary Nerve Area of Anesthesia

Infraclavicular Area of Anesthesia

Infraclavicular Area of Anesthesia

Popliteal Sciatica Area of Anesthesia
Suprainguinal Nerve Block
An 89 year old male presented after a mechanical fall onto his right hip. X-rays demonstrated a comminuted right intertrochanteric fracture.
An ultrasound-guided fascia iliaca block can be performed using the suprainguinal approach when placing the probe perpendicular to the inguinal ligament. The internal oblique (cephalad, blue) and the sartorius (caudad, red) muscles are encompassed by the fascia lata (green) superiorly and the fascia iliaca (yellow) inferiorly. These two come together to form a “bow tie” as shown above, anesthetic is deposited below the fascia iliaca. Studies have shown improved analgesia with the suprainguinal, as it is believed to have a higher likelihood of blocking the lateral femoral cutaneous nerve and the obturator nerve.
Sanna Ho-Gotshall, DO, Ultrasound Fellow
Casey Wilson, MD, Ultrasound Director, Emergency Medicine Program Director
Ulnar Nerve Block
Ulnar nerve block done in plane. Provides excellent anesthetic for isolated hand injuries. In this case, allowed for faster time to repair and avoided use of ketamine sedation. Inject in place and use small amounts of lidocaine to make sure you are in the correct space before bathing the nerve with the entire amount of anesthetic.
Julia Brant, Pediatric Emergency Medicine Fellow
@pedipocus
Median Nerve Block
15 y/o M "fell into a mirror," landing on his hand and suffering multiple, complicated lacerations at the base of his second digit with the tendon showing. Instead of injecting local anesthesia throughout, a simple median nerve block was done under POCUS guidance. In plane technique. One stick. One happy patient.
Matthew Riscinti, MD - Kings County/SUNY Downstate Emergency Medicine
Radial Nerve Block
Notice here in a still-shot of a radial nerve block, you can visually appreciate the infiltration of local anesthetic as evidenced by the hypoechoic area surrounding the radial nerve.
Aaron Inouye, PA-C North Canyon Medical Center
@PAintheED
Interscalene Block - High Speed
80 y/o intoxicated female found down with L shoulder dislocation. In order to avoid opiates/sedatives, inter-scalene block was done to facilitate reduction.
http://highlandultrasound.com/interscalene-block - for more on technique
Dr. Forrest Andersen - Denver Health Emergency Medicine
Interscalene Block
80 y/o intoxicated female found down with L shoulder dislocation. In order to avoid opiates/sedatives, inter-scalene block was done to facilitate reduction.
http://highlandultrasound.com/interscalene-block - for more on technique
Dr. Forrest Andersen - Denver Health Emergency Medicine
Median Nerve
The median nerve is the most echogenic of the upper extremity nerves. It is also the only forearm nerve that that does not run alongside vessels, making it an easy and safe target for a nerve block. It is seen here as a hyperechoic, honeycomb appearing oval in the center of the screen. The probe is positioned in transverse orientation on the volar aspect of the forearm.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Radial Nerve
The radial nerve is the least echogenic of the upper extremity nerves, and can be difficult to visualize. It is located lateral (radial) to the radial artery. It is best seen by following the radial artery in transverse proximally up the arm; eventually a bright hyperechoic oval will be visible traveling away from the artery. (right arm seen here)
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Ulnar Nerve (Copy)
The ulnar nerve is located medial (ulnar) to the ulnar artery. It is best seen by following the ulnar artery in transverse proximally up the arm; eventually a bright hyperechoic triangle will be visible traveling away from the artery. (left arm seen here)
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Ulnar Nerve and Artery
The ulnar artery with color doppler showing pulsatile flow, and the bright hyperechoic ulnar nerve visible to the left of the screen. Remember, the ulnar nerve is always “ulnar” to the ulnar artery.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Median Nerve Injection
55 y/o female with recurrent carpal tunnel symptoms not improved with conservative management. Benefits of US guidance include vessel avoidance, and needle placement for surrounding median nerve with steroid solution.
Dr. Magner
Radial Nerve Block
Radial Nerve Block
Performed for wound exploration and laceration repair of a 1.5cm laceration located at the radial aspect of the forearm, proximal 4cm from the radial styloid. The nerve was identified as a heterogenous hyperechoic structure lateral to the radial artery and superficial to the radius. Located superior is the extensor carpi radialis longus and brevis muscle. Hydrodissection was performed in-plane using a 22-gauge needle with 5mL of 1% lidocaine without epinephrine.
Submitted by Dr. Spencer Kim and Dr. Maurelus, Kings County Medical Center
Posterior Tibial Nerve Block
Posterior Tibial Nerve Block
Foot and heel pain after missing a jump while skiing. XR showed calcaneal fracture. Pain not relieved by IV analgesics, posterior tibial nerve performed proximal to medial malleolus with complete resolution of pain. Nerve seen inferior to artery. Watch as fluid surrounds nerve. Use in-plane approach to avoid vasculature and avoid intraneural injection.
Submitted by Dr. Miguel Agrait Gonzalez, University of Puerto Rico
Popliteal Sciatic Nerve Block
Popliteal Sciatic Nerve Block
A 71 year old woman with dementia and mobility constraints presented with a gaping laceration over the posterior gastrocnemius extending inferiorly towards the achilles after a “fall from wheelchair”. Achilles tendon function was preserved and the wound was explored without foreign body. The patient did not tolerate initial attempts at laceration repair after local anesthesia due to pain and anxiety.
A decision was made to perform a popliteal sciatic nerve block.
The patient was placed in the prone position and 1% lidocaine without epi was drawn up in a syringe with extension tubing connected to a spinal needle under sterile conditions. A linear probe was used to identify the sciatic nerve just below the adductor magnus muscle. Lidocaine was injected 1 cm distal to the sciatic nerve’s bifurcation into the Common Peroneal N. and Tibial N. using the “in-plane” view. 20mL spread above, below and around the sciatic nerve sheath was sufficient to provide near-complete anesthesia and the patient tolerated the entire laceration repair.
Submitted by Dr. Jordan Dow and Dr. Kelly Maurelus, Kings County Medical Center
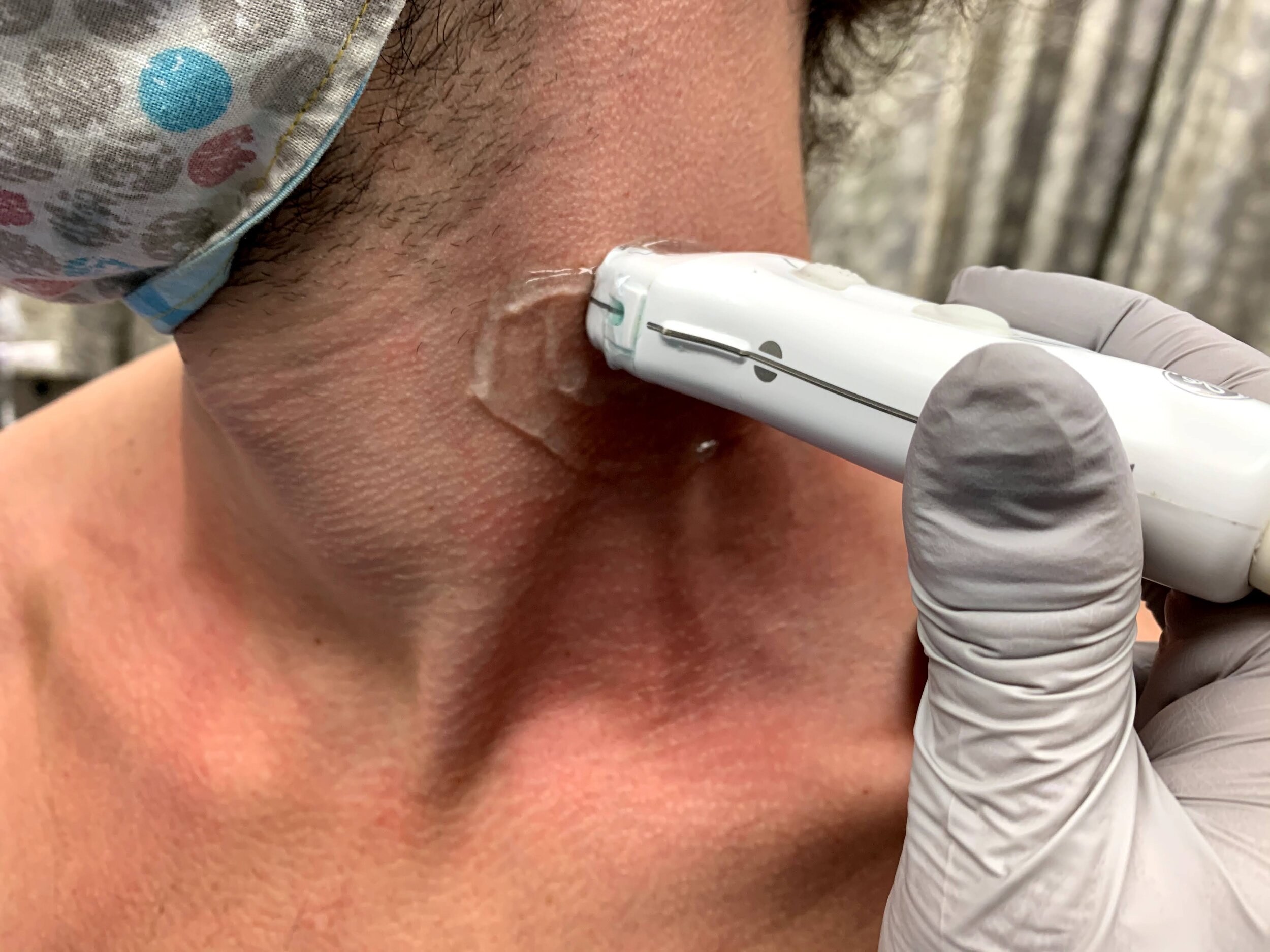
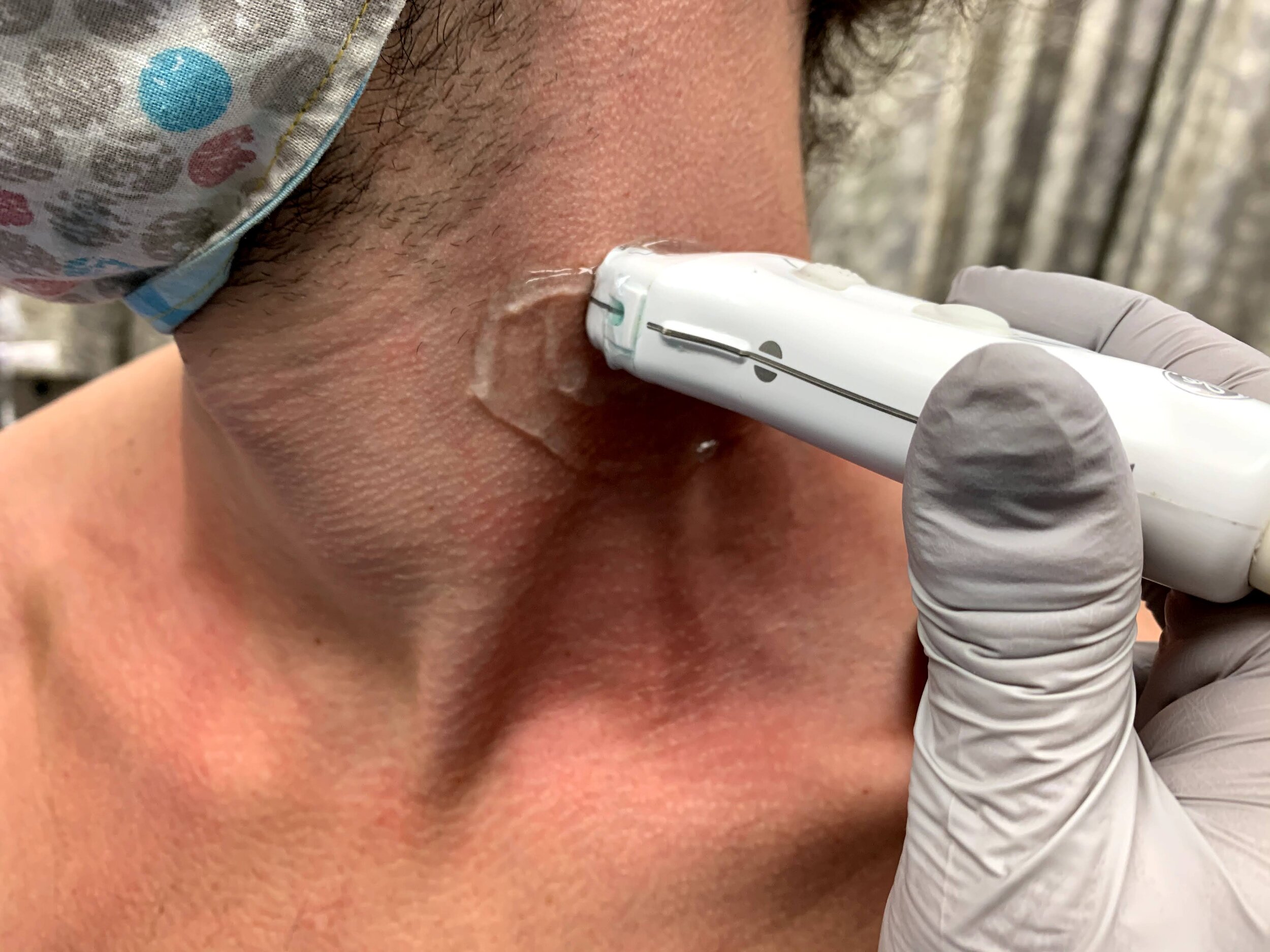
Superficial Cervical Plexus Block
The superficial cervical plexus block pictured above was utilized in an elderly awake patient with dementia for the placement of an IJ CVC. Other indications include I&Ds of submandibular abscesses, lac repair to the ear lobe, and clavicular fractures. The block is best performed in-plane so as to directly visualize the dissection of the plane between the Sternocleidomastoid muscle (visualized superiorly) and the scalene muscles (visualized inferior to the needle insertion), and works by bathing several nerve branches at once. The area of anesthetic overlies the sternocleidomastoid muscle from the clavicle up to the preauricular space and oddly enough, includes the earlobe.
Authored by Dr. Nicole Anthony and Dr. Kelly Maurelus, Kings County Medical Center
Femoral Nerve Block
Demonstration of an in-plane femoral nerve block, with needle seen entering from lateral to medial, depositing anesthetic in the space just lateral to the femoral nerve (*).
This block was performed in a 50s year-old male patient with an intertrochanteric femur fracture, with successful analgesia until surgery was performed the next day.
Drs. Kathleen Joseph, PGY-2 and Reid Haflich, PGY-4
Denver Health Residency in Emergency Medicine
Radial Nerve Block at the Elbow
Demonstration of an in-plane radial nerve block, with needle shown entering from the radial aspect, depositing anesthetic deep and radial to the radial nerve (*).
Dr. Claudia Quenelle, PGY-3
Denver Health Residency in Emergency Medicine
Interscalene Brachial Plexus Block
In-plane interscalene block, with needle entering from screen right (lateral and posterior), showing injection of anesthetic within the interscalene groove, surrounding the brachial plexus (*). The subclavian artery can be seen pulsating screen left (medial) to the brachial plexus.
Denver Health Ultrasound Fellowship Archive
Common Peroneal Block
In-plane common peroneal nerve block at the level of the proximal fibula. The needle is seen first contacting the common peroneal nerve (*), then injecting anesthetic within the nerve perineurium.
Denver Health Ultrasound Fellowship Archive
Tibial Nerve Block
In-plane tibial nerve block, with needle seen entering from screen right (posterior), with injection of anesthetic superficial to the tibial nerve (*). The posterior tibial artery can be seen pulsating screen left of (anterior to) the nerve.
Denver Health Ultrasound Fellowship
Common Peroneal Block
In-plane common peroneal nerve block, with needle entering from the medial aspect. Sequential injection of anesthetic, eventually injecting superficial to common peroneal nerve (*). The proximal fibula cortex is visible at bottom of screen left.
Denver Health Ultrasound Fellowship Archive
Ulnar Nerve Block 2
In-plane ulnar nerve block, with needle seen entering from screen right (ulnar aspect), with anesthetic sequentially deposited deep, lateral, then superficial to ulnar nerve (*). The ulnar artery can be seen pulsating to the left of (radially to) the ulnar nerve.
Denver Health Ultrasound Fellowship Archive
Ulnar Nerve Block 3
In-plane ulnar nerve block with needle entering from screen left (ulnar aspect). Demonstration of successful block with anesthetic located deep to ulnar nerve (*). The ulnar artery can be seen pulsating to screen right of (radial to) the nerve.
Denver Health Ultrasound Fellowship Archive
Median Nerve Block 1
In-plane median nerve block at the wrist, with needle seen entering from screen right, with anesthetic deposited adjacent to median nerve (*).
Denver Health Ultrasound Fellowship
Median Nerve Block 2
Out-of-plane median nerve block, with needle seen entering directly above median nerve, with anesthetic deposited superficial to median nerve (*).
Denver Health Ultrasound Fellowship Archive
Median Nerve Block 3
In-plane median nerve block, with needle seen entering from screen right (ulnar aspect), with anesthetic deposited deep to median nerve (*). the radial artery can be seen pulsating superficial to and screen left of (radial to) the nerve.
Denver Health Ultrasound Fellowship
Median Nerve Block 4
Out-of-plane median nerve block, with needle seen entering just above the nerve, with anesthetic deposited superficial to median nerve (*).
Denver Health Ultrasound Fellowship
Median Nerve Block 5
Out-of-plane median nerve block, with needle seen entering directly above the nerve and depositing anesthetic superficial to median nerve (*). The distal radius cortex can be seen at the lower left of the image (deep and radial to the nerve).
Denver Health Ultrasound Fellowship Archive
Ulnar Nerve Block 4
In-plane ulnar nerve block, with needle seen entering from screen right (radial aspect), with anesthetic deposited superficial to ulnar nerve (*). The ulnar artery can be seen pulsating screen right of (radial to) the nerve.
Denver Health Ultrasound Fellowship Archive
Ulnar Nerve Block 5
In-plane ulnar nerve block with needle seen entering from the ulnar aspect, depositing anesthetic first in soft tissues, followed by injection adjacent to the ulnar nerve (*). The ulnar artery can be seen pulsating screen left (radial to) the nerve.
Denver Health Ultrasound Fellowship Archive
Ulnar Nerve Block 6
In-plane ulnar nerve block, with needle seen entering from screen right (ulnar aspect), with anesthetic deposited superficial/adjacent to ulnar nerve (*). The ulnar artery can be seen pulsating screen left of (radial to) the nerve.
Denver Health Ultrasound Fellowship Archive
Interscalene Anatomy
Localization and view of the brachial plexus nerve roots (*) in the interscalene groove. The right of screen is anterior/medial and left of screen is lateral/posterior. The carotid artery (A) and internal jugular vein (V) can be seen anterior and medially to the brachial plexus.
Dr. Nick Aunchman
University of Vermont Medical Center
Ulnar Nerve Block 7
In-plane ulnar nerve block with needle entering from ulnar aspect, with anesthetic surrounding ulnar nerve. the ulnar artery (A) can be seen pulsating radially to the nerve.
Dr. Peter Weimersheimer
University of Vermont Medical Center
Fascia Iliaca
"74 male presenting with mechanical fall down twelve steps complaining primarily of severe right hip pain. X-ray demonstrating comminuted subcapital femoral neck fracture with significant angulation. In agreement with orthopedic recommendations an ultrasound-guided fascia iliaca nerve block was performed with 40cc of bupivacaine 0.25% with successful analgesia.
Transverse views of the right femoral artery and vein are first identified (not shown), then translocated laterally to identify the fascia iliaca plane. Sartorius and iliacus muscles are seen above and below, respectively. An ultrasound-guided longitudinal view was utilized to introduce the needle immediately below the fascia iliaca plane and administer anesthetic."
Authored by Dr. Chris Lim, Kings County Medical Center
Serratus Anterior Plane Block
80s F presented with a mechanical fall, found to have multiple rib fractures and subsequent poor incentive spirometry. An in-plane serratus anterior plane block was performed on the affected side using the linear transducer in a transverse plane orientation at the level of the 4th/5th rib at the mid axillary line. Local anesthetic can be seen spreading in the fascial plane between serratus anterior (deep) and latissimus dorsi (superficial) muscles. The lung pleura can be seen sliding below serratus anterior. The patient reported relief soon after the block.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Radial Nerve Block at the Elbow
50s M with PMH IVDU presented with a dorsal hand abscess. To facilitate I&D, a radial nerve block was performed at the level of the elbow using the linear transducer and an in-plane approach. Injection of anesthetic seen adjacent to the radial nerve (*). The hyperechoic distal humeral cortex can be seen at the right of the image. Shortly after the block, I&D was able to be performed at bedside.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Axillary Brachial Plexus Anatomy
Demonstration of the axillary brachial plexus as seen in transverse view with the linear transducer at the level of the proximal humerus. The brachial plexus (*) can be seen medial to the pulsating axillary artery. The musculocutaneous nerve (^) can be seen lateral to the artery/brachial plexus, deep to the biceps muscle and superficial to the coracobrachialis muscle.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Infraclavicular Brachial Plexus Anatomy
Demonstration of the anatomy of the infraclavicular brachial plexus with the linear transducer in a parasagittal orientation just lateral to the mid-clavicular line. The pulsating subclavian artery can be seen surrounded by the brachial plexus (*). The hyperechoic clavicle is seen in short axis at the right of the image. Sliding pleura can be seen deep to the artery/brachial plexus.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Interscalene Brachial Plexus Anatomy
Demonstration of the anatomy of the brachial plexus in the interscalene groove. The C5-7 nerve roots (*) can be seen between the anterior and middle scalene muscles at the right (lateral/posterior) aspect of the image. The posterior edge of the sternocleidomastoid muscle is seen superficial and left of the image.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Common Peroneal Nerve Anatomy
Demonstration of the anatomy of the common peroneal nerve at the level of the proximal fibula. This image was obtained with the linear transducer placed in a transverse orientation on the lateral aspect of the fibular head. The nerve (*) is seen just superficial to the hyperechoic fibular cortex.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Sciatic Nerve Anatomy
Anatomy of the sciatic nerve in the popliteal fossa. This image was obtained using the linear transducer in a transverse orientation in the popliteal fossa. The sciatic nerve (*) can be seen superficial to the pulsating popliteal artery, just superficial to the partially compressed popliteal vein. The hyperechoic femoral condylar cortex can be seen at the left of the image.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Tibial Nerve Anatomy
Anatomy of the tibial nerve as it passes posterior of the medial malleolus. The image was obtained using the linear transducer in a transverse orientation just posterior to the medial malleolus. The nerve (*) is seen posterior to (right of) the pulsating posterior tibial artery. Also seen is the hyperechoic malleolar cortex of the distal tibia at the bottom of the image, as well as the tendons of tibialis posterior and flexor digitorum longus anterior to (left of) the artery and nerve.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Serratus Anterior Anatomy
Anatomy of the serratus anterior, as obtained using a linear transducer in a transverse orientation at the level of the 4th/5th rib in the mid axillary line. Anterior is at the left of the image. The latissimus dorsi muscle is seen most superficially, with the serratus anterior muscle deep to it, just above the hyperechoic ribs. Sliding pleura can be seen below the ribs. The thoracodorsal artery can be seen pulsating in the fascial plane between latissimus dorsi and serratus anterior.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine

Superficial Cervical Plexus Anatomy
Demonstration of the anatomy of the superficial cervical plexus. The posterior border of the sternocleidomastoid muscle is seen at the center left of screen, and the target fascial plane for a superficial cervical plexus nerve block is highlighted (*). The pulsating carotid artery is seen at the anterior aspect of the image.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Supraclavicular Brachial Plexus Anatomy
Anatomy of the supraclavicular brachial plexus. This image was obtained with the linear transducer in a parasagittal orientation just lateral to the neck. Left of image is anterior in this view. The brachial plexus (*) is seen just posterior to the pulsating subclavian artery. The hyperechoic first rib can be seen just below the artery and brachial plexus.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Thoracic Vertebral Anatomy
Anatomy of a thoracic vertebra as seen in transverse view, using the linear transducer. The spinous process (SP) is seen most superficially and in the midline, with the lamina (L) seen connecting the spinous process to the transverse process (TP) laterally. Sliding pleura can also be seen lateral and deep to the transverse process.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Serratus Anterior Plane Block 2
60s F presented to the ED three days after a fall at home, complaining of right chest pain, and was found to have multiple rib fractures on CT with a small amount of hemothorax and blood in the horizontal fissure. A serratus anterior plane block was performed using an in-plane approach to inject anesthetic in the fascial plane between the pectoralis minor (PM) and serratus anterior (SA) muscles. Fluid can be seen in the pleural space beneath serratus anterior. 30 minutes after the nerve block, the patient was feeling much improved, her performance on incentive spirometry improved markedly, and she requested discharge.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Sub-Serratus Anterior Plane Block
60s F presented to the ED three days after a fall at home, complaining of right chest pain, and was found to have multiple rib fractures on CT with a small amount of hemothorax and blood in the horizontal fissure. A serratus anterior plane block was performed using an in-plane approach to inject anesthetic in the fascial plane between the pectoralis minor and serratus anterior muscles (not shown), followed by this injection into the fascial space between the rib and serratus anterior. Additionally, fluid (likely blood) can be seen here in the pleural space below the rib. 30 minutes after the nerve block, the patient was feeling much improved, her performance on incentive spirometry improved markedly, and she requested discharge.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Erector Spinae Anatomy Scan
Dynamic view of the anatomy of the erector spinae block. This view is obtained using the linear transducer in a sagittal orientation. The clip starts in the midline, and a pinpoint hyperechoic thoracic spinous process is briefly seen. As the probe is swept laterally, broad hyperechoic transverse processes are seen, with the erector spinae muscles just superficial to these. Further laterally, the transverse processes disappear and broad hyperechoic ribs come into view, with sliding pleura visible underneath. Notice the lack of visible pleura when transverse processes are in view. The erector spinae block is performed in the plane viewing transverse processes, without ribs/pleura visible.
Drs. Sam Paskin-Flerlage, PGY4 and Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Neonatal Fascia Iliaca Block
A 50 day-old male was transferred from an outside hospital with concern for NAT after skeletal survey showed old rib fractures, and a significantly displaced and angulated femoral midshaft fracture. A ultrasound-guided fascia iliaca block was performed to aid with passive reduction while in a Pavlik harness. Anesthetic spread can be seen along the fascial plane just superior to the femoral nerve (*). The pulsating femoral artery is seen medial (left of screen) to the nerve. The patient had pain relief with the block, and follow up radiographs showed better reduction after being in the harness without manual manipulation.
Dr. Michael Heffler, PGY3, Denver Health Residency in Emergency Medicine
Dr. Emily Greenwald, 3rd year PEM fellow, Children’s Hospital Colorado
Dr. Megan Mickley, PEM Attending Physician, co-director Pediatric Emergency Ultrasound, Children’s Hospital Colorado
Superficial Cervical Plexus Block
40s F presented to the ED with left shoulder pain after a fall out of bed 1 day prior to arrival. She was found to have a closed, displaced and comminuted fracture of the distal clavicle, which was managed non-operatively with a sling. A superficial cervical plexus nerve block was performed for analgesia. This clip shows the block being performed with an in-plane technique, with the needle entering posteriorly/laterally (screen right), to instill local anesthetic along the fascial plane (*) just deep to the sternocleidomastoid muscle. The carotid artery can be seen pulsating medially (left of screen). The patient had significant improvement of her pain after the block, and was discharged.
Drs. Anna Engeln and Matt Riscinti
Denver Health Medical Center
Radial Nerve Block
Notice here in a still-shot of a radial nerve block, you can visually appreciate the infiltration of local anesthetic as evidenced by the hypoechoic area surrounding the radial nerve.
Aaron Inouye, PA-C North Canyon Medical Center
@PAintheED
Interscalene Block - High Speed
80 y/o intoxicated female found down with L shoulder dislocation. In order to avoid opiates/sedatives, inter-scalene block was done to facilitate reduction.
http://highlandultrasound.com/interscalene-block - for more on technique
Dr. Forrest Andersen - Denver Health Emergency Medicine
Interscalene Block
80 y/o intoxicated female found down with L shoulder dislocation. In order to avoid opiates/sedatives, inter-scalene block was done to facilitate reduction.
http://highlandultrasound.com/interscalene-block - for more on technique
Dr. Forrest Andersen - Denver Health Emergency Medicine
Median Nerve Block
15 y/o M "fell into a mirror," landing on his hand and suffering multiple, complicated lacerations at the base of his second digit with the tendon showing. Instead of injecting local anesthesia throughout, a simple median nerve block was done under POCUS guidance. In plane technique. One stick. One happy patient.
Matthew Riscinti, MD - Kings County/SUNY Downstate Emergency Medicine
Median Nerve Injection
55 y/o female with recurrent carpal tunnel symptoms not improved with conservative management. Benefits of US guidance include vessel avoidance, and needle placement for surrounding median nerve with steroid solution.
Dr. Magner
Radial Nerve Block at the Elbow 2
20s F presented with large complex laceration to the distal forearm after an assault. Ultrasound radial and median nerve blocks were performed at the elbow to facilitate washout and closure. This clip illustrates the radial nerve block, where the needle is entering from the posterolateral aspect of the upper arm, and anesthetic can be seen surrounding the radial nerve (*).
Dr. Gabe Siegel
Denver Health Residency in Emergency Medicine
Median Nerve Block at the Elbow
20s F presented with large complex laceration to the distal forearm after an assault. Ultrasound radial and median nerve blocks were performed at the elbow to facilitate washout and closure. This clip illustrates the median nerve block, where the needle is entering from the lateral/radial aspect of the upper arm, and anesthetic can be seen adjacent to the median nerve (*).
Dr. Gabe Siegel
Denver Health Residency in Emergency Medicine
Popliteal Sciatic Nerve Block
30s M presented to the ED with a large anterior shin wound after being struck by a car. A popliteal sciatic nerve block was performed for analgesia with good effect, and the patient was able to have his wound irrigated and repaired. In this clip, the sciatic nerve (*) is first seen superficial to the pulsating popliteal artery, and then anesthetic can be seen being injected within the sciatic nerve sheath (Vloka’s sheath).
Dr. Sabrina Kaplan, PGY3
Denver Health Residency in Emergency Medicine
Fascia Iliaca Nerve Block
An elderly female with multiple medical comorbidities presented to the ED with hip and thigh pain after a fall at home. Imaging demonstrated an intertrochanteric proximal femur fracture, and, after consultation with Orthopedic Surgery and detailed documentation of the patient’s neurovascular exam, a fascia iliaca nerve block was performed. This clip demonstrates the block, where the needle can be seen entering from the left of screen (laterally) along the trajectory outlined by the yellow diagonal, and anesthetic can be seen infusing just deep to the fascia iliaca and superomedially to the iliacus muscle. The pulsating femoral artery is seen medial to the site of injection. After the nerve block, the patient’s pain was improved and she was admitted for surgical fixation the next morning.
Dr. Arian Anderson, PGY-4 and Dr. Michael Heffler, PGY-3
Denver Health Residency in Emergency Medicine
Fascia Iliaca Block 2
A 60s F presented to the ED with hip/leg pain after a mechanical slip and fall. She had an obvious closed deformity of the proximal femur on exam, and radiographs demonstrated an intertrochanteric femur fracture with subtrochanteric extension. After consultation with orthopedic surgery, a fascia iliaca block was performed to provide analgesia and to facilitate traction radiographs, and she was admitted for surgery. This clip shows the block being performed, with the needle entering from left of screen (laterally), depositing anesthetic just deep to the fascia iliaca, superficial to the iliacus muscle. The femoral artery and vein can be seen to the right (medial) of the area of injection.
Dr. Arian Anderson, PGY4, and Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Fascia Iliaca Nerve Block for Femur Fracture
A 20s F was brought in by ambulance after she was struck by a vehicle. She had an obvious closed deformity to her thigh. Initial trauma workup was negative for other injuries, she remained awake/alert and hemodynamically stable, and was neurovascularly intact distally. After orthopedic consultation, a fascia iliaca nerve block was performed for analgesia in preparation for distal femur traction pin placement. The needle here enters from left of screen (lateral), injecting anesthetic just deep to the fascia iliaca, and spreading adjacent to the femoral nerve, which is seen to the left of (lateral to) the pulsating femoral artery. The patient had improvement of her pain, traction pinning was performed, and she was admitted for surgery.
Dr. Arian Anderson, PGY4
Denver Health Residency in Emergency Medicine
Fascia Iliaca Nerve Block Anatomy
This clip shows the normal anatomy seen during a fascia iliaca nerve block. The image is obtained using a linear transducer in a transverse orientation over the middle to lateral third of the inguinal ligament. The probe marker is to the lateral aspect of the patient. The femoral nerve (N) is seen lateral to the femoral artery (A), and the sartorius muscle (S) is seen superficial to the iliacus muscle (I), with the fascia iliaca in between the two muscles. The target site for injection is just deep to the fascia iliaca, at a point lateral to the femoral nerve (*). Anesthetic should be visualized tracking medially toward the femoral nerve.
Dr. Arian Anderson, PGY4
Denver Health Residency in Emergency Medicine
Ulnar Nerve
The ulnar nerve is located medial (ulnar) to the ulnar artery. It is best seen by following the ulnar artery in transverse proximally up the arm; eventually a bright hyperechoic triangle will be visible traveling away from the artery. (left arm seen here)
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Ulnar Nerve and Artery
The ulnar artery with color doppler showing pulsatile flow, and the bright hyperechoic ulnar nerve visible to the left of the screen. Remember, the ulnar nerve is always “ulnar” to the ulnar artery.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Median Nerve
The median nerve is the most echogenic of the upper extremity nerves. It is also the only forearm nerve that that does not run alongside vessels, making it an easy and safe target for a nerve block. It is seen here as a hyperechoic, honeycomb appearing oval in the center of the screen. The probe is positioned in transverse orientation on the volar aspect of the forearm.
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Radial Nerve
The radial nerve is the least echogenic of the upper extremity nerves, and can be difficult to visualize. It is located lateral (radial) to the radial artery. It is best seen by following the radial artery in transverse proximally up the arm; eventually a bright hyperechoic oval will be visible traveling away from the artery. (right arm seen here)
Hannah Kopinksi and Dr. Lindsay Davis - NYU Emergency Medicine
Pediatric Fascia Iliaca Nerve Block
A teenage female patient arrived to the ED via EMS after she was truck by a car, sustaining multiple serious injuries, including a midshaft femur fracture which was significantly displaced. She required multiple rounds of IV analgesics, so a fascia iliaca block was performed to augment pain control. Shown here, the needle is seen entering from the lateral aspect through the iliacus muscle, injecting anesthetic just deep to the fascia iliaca. The femoral artery and vein are seen medial to this at the left of the image. The patient had improvement in pain level, and was able to be admitted to the ICU for further care.
Dr. Kate Simeon, PGY1, and Dr. Nik Matsler, PGY4
Denver Health Residency in Emergency Medicine

Radial Nerve Probe Location
Radial Nerve Probe Location
Interscalene Nerve Block
20s M with PMH recurrent shoulder dislocation presented with shoulder pain and concern for dislocation. Radiographs confirmed anterior glenohumeral dislocation and showed a Hill-Sachs deformity. An interscalene brachial plexus block was performed for analgesia. The block is shown here, with the needle entering from the lateral aspect or left of screen, injecting anesthetic adjacent to the nerve roots (*) within the interscalene groove. The patient had good pain control with the block, allowing easy bedside reduction without additional parenteral medications or conscious sedation. Repeat radiographs confirmed adequate reduction of the dislocation and the patient was discharged with orthopedic follow up.
Dr. Molly Thiessen
Denver Health Medical Center
Serratus Anterior Plane Block for Chest Tube Placement
20s F presented with chest pain after a trigger point injection to the back at a chiropractic appointment, found to have a large pneumothorax. To facilitate analgesia for chest tube placement, a serratus anterior plane block was performed under ultrasound guidance. Seen here, the needle is entering from the posterior aspect, and deposits anesthetic in the plane between serratus anterior and latissimus dorsi. The patient had improved pain and was able to have a tube thoracostomy performed, and she was admitted for further observation.
Dr. Mark Serpico, PGY3 and Dr. Molly Thiessen, Ultrasound Fellowship Director
Denver Health Residency in Emergency Medicine
Interscalene Nerve Root Anatomy
30s M presented with shoulder dislocation. To facilitate reduction, an interscalene nerve block was performed. This clip demonstrates the brachial plexus nerve roots (*) as seen just outside of the interscalene groove - the middle scalene muscle is seen just deep to the nerve roots, with the sternocleidomastoid muscle seen superficial to these. The patient had onset of anesthesia after the block and was able to have closed reduction performed in the ED.
Dr. Olivia Serigano, PGY3
Denver Health Residency in Emergency Medicine
Superficial Cervical Plexus Block for Clavicle Fracture
30s M presented with clavicle pain after fall on bike, noted to have obvious deformity to L clavicle, and to be closed and neurovascularly intact. Radiographs confirmed a distal third clavicle fracture, and nonoperative management was recommended by orthopedic surgery. To augment pain control, a superficial cervical plexus block was performed. In these images, the needle is seen entering from the posterior aspect (left of screen), depositing anesthetic in the plane just deep to the sternocleidomastoid muscle (*). The patient had improvement of pain and was discharged with outpatient orthopedic follow up.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Popliteal Sciatic Nerve Block
30s M presented with foot pain after an accidental injury from a lawn mower blade. Found to have a large laceration and open metatarsal fracture. A popliteal sciatic nerve block was performed for pain control overnight while the patient awaited surgery the next morning. The block is shown here, with the needle entering from the lateral aspect (right of screen), injecting anesthetic adjacent to the sciatic nerve (*) in the popliteal fossa. The patient had improved pain control and was admitted for surgery.
Megan Foy, MS4, University of Colorado School of Medicine
Dr. Adam Esch, PGY4, Denver Health Residency in Emergency Medicine
Fascia Iliaca Block for Distal Femur Fracture
70s F presented with lower extremity pain after a mechanical trip and fall on the stairs. She arrived with a closed deformity of the distal thigh, and radiographs confirmed a comminuted distal femur fracture. A fascia iliaca block was performed for analgesia and to facilitate traction pinning. The block is shown here, with the needle entering from the lateral aspect (screen right) and depositing anesthetic just deep to the fascia iliaca (*) which lies deep to the sartorius muscle and superficial to the iliacus muscle. The patient had significant relief soon after the block and was able to be admitted for surgery.
Dr. Michael Heffler, PGY3, Dr. Spencer Tomberg, Attending
Denver Health Residency in Emergency Medicine
Interscalene Anatomy
This clip demonstrates the anatomy of the brachial plexus in the interscalene groove. The anterior scalene (AS) and middle scalene (MS) muscles are seen, with the brachial plexus nerve roots (*) seen in the interscalene groove. Color doppler is used to highlight the carotid artery (red) and internal jugular vein (blue) which lie medial/anterior to the brachial plexus. Color doppler is also useful to verify that the brachial plexus nerve roots are not lying deep to other blood vessels.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Interscalene
30s M with past medical history of recurrent shoulder dislocations who had failed prior surgery presented with anterior shoulder dislocation. An interscalene nerve block was performed for analgesia to facilitate reduction. After confirmation and documentation of intact neurovascular exam, the nerve block was performed as shown. The needle is seen entering from the posterior aspect (left of screen), and is instilling local anesthetic which surrounds the brachial plexus (*). The patient had significantly improved pain after the nerve block but ultimately did require further sedation to overcome muscle spasm in order to facilitate successful reduction.
Dr. Michael Heffler, PGY3
Denver Health Residency in Emergency Medicine
Posterior Tibial Nerve Block
A 20s y/o patient presented after a laceration to the plantar surface of the foot from glass. After exclusion of retained foreign body by XR and physical exam, the laceration was irrigated and repaired using local infiltration of anesthesia, and the patient was discharged. The patient re-presented to the ED within a few hours with continued pain. The laceration repair was intact, and a posterior tibial nerve block was performed for analgesia. This clip shows the nerve block being performed. The linear probe was placed in a transverse plane, just posterior to the medial malleolus, over the “tarsal tunnel.” The left of this image is anterior, and the right is posterior. The needle (^) can be seen entering from the posterior aspect, infiltrating anesthetic around the tibial nerve (*). The pulsating posterior tibial artery is seen anterior to the nerve.
The anatomy of the tarsal tunnel can be recalled by the mnemonic “Tom, Dick, And Very Nervous Harry,” which lists the structures in order of anterior to posterior (tibialis posterior tendon, flexor digitorum longus tendon, posterior tibial artery, posterior tibial vein, tibial nerve, flexor hallucis longus tendon), however the tendons and posterior tibial vein are less well seen in this clip.
Dr. James Sutton, PGY-3
Denver Health Residency in Emergency Medicine
Interscalene Brachial Plexus Nerve Block
20s M with history of recurrent shoulder dislocation presented with shoulder pain and suspected dislocation. He was found to be neurovascularly intact, and after confirmation of dislocation with POCUS and XR, an interscalene nerve block was performed to facilitate reduction. The block is shown here, where the needle is seen entering from the posterior/lateral aspect at the left of screen, injecting anesthetic between the middle and anterior scalene muscles, adjacent to the brachial plexus nerve roots (*). The patient had relief of pain within minutes and was able to be reduced at the bedside without complication.
Dr. Ian Eisenhauer, PGY-1
Denver Health Residency in Emergency Medicine
Superficial Cervical Plexus Probe Placement

Erector Spinae Anterior Area

Erector Spinae Posterior Area

Ulnar Probe Position at Elbow
Supraclavicular Nerve Block Anatomy
This is an ultrasound clip demonstrating the anatomy for a supraclavicular nerve block. The probe is placed parallel to and just superior to the clavicle. The subclavian artery can be seen pulsating in the middle of the screen just superior to the hyperechoic cortex of the first rib. The * denotes the large brachial plexus bundle which can be seen just lateral to the artery. Pleural sliding can also be appreciated on both sides of the rib.
Michael Macias
Infraclavicular Brachial Plexus Block Anatomy
This is an ultrasound clip demonstrating the anatomy for an infraclavicular block. The probe is placed in a parasagittal orientation just medial to the coracoid process and inferior to the clavicle. The axillary artery can be seen pulsating in the middle of the screen. The * denotes the three cords of the the brachial plexus at this location (lateral, medial, and posterior). Two muscles layers can be seen at the top of the screen, pec major and the underlying pec minor.
Michael Macias
Posterior Tibial Nerve Block for Heel Wounds
30s M presented with foot pain after his foot was run over by a car while he was riding a moped. He had lacerations over the plantar aspect of his foot without underlying fracture on XR. To facilitate wound irrigation and dressing, a posterior tibial nerve block was performed. The block is shown here, with the medial malleolus just out of view to the right of the image. The needle approaches in plane from the posterior aspect, and deposits anesthetic adjacent to the posterior tibial nerve (*). The posterior tibial artery is seen pulsating just anterior (right of screen) to the nerve. The patient had anesthesia achieved and his wounds were able to be irrigated and dressed.
Dr. Carleigh Benton, PGY-4
Denver Health Residency in Emergency Medicine

Supraclavicular Probe Placement

Infraclavicular Probe Placement
Supraclavicular Nerve Block
In plane supraclavicular nerve block used for pain management in a patient with a mid shaft humerus fracture. Spread of anesthetic can be seen around the brachial plexus bundle (*).
Michael Macias
Erector Spinae Plane Block
60s M presented after bicycle crash, and was found to have multiple unilateral rib fractures. To aid with pain control, an erector spinae plane block was placed using bupivacaine. The block is shown here, with the needle approaching in plane from the right of the screen (inferior). The first few seconds of the clip show the anatomy from lateral to medial, with the posterior rib with associated pleura seen, before the more medial transverse process is seen, without associated pleura. The target of anesthetic spread is the fascial plane (*) between the transverse process and the overlying erector spinae muscle. The second half of the clip shows administration of anesthetic with spread visible along the target fascial plane.
Dr. Matthew Riscinti, Fellowship Director
Denver Health Ultrasound
Sub-Serratus Anterior Plane Block for GSW
20s M presented after GSW to the chest, and sustained a hemothorax requiring non-emergent chest tube placement. To augment pain control, a serratus anterior plane block was performed with bupivacaine. The block is shown here, with infiltration of the hypoechoic anesthetic deep to the serratus anterior muscle, just above the rib and intercostal muscles. Anesthetic could alternatively be placed in the fascial plane between serratus anterior and latissimus dorsi, which is the fascial plane seen superficial to the anesthetic in this clip. This patient was able to have a chest tube placed with adequate analgesia and without complication and was admitted for further management of his GSW.
Dr. Olivia Serigano, PGY4
Denver Health Residency in Emergency Medicine
Supraclavicular Brachial Plexus Block
40s M presented with shoulder pain after a fall at work, and radiographs confirmed a proximal humerus fracture. As the patient was neurovascularly intact and had a closed fracture, conservative management in a sling was planned by orthopedic surgery. To augment pain control, a supraclavicular brachial plexus block was performed using bupivacaine and dexamethasone. The block is shown here, with color doppler first used to identify the carotid artery and confirm the absence of vascular flow in the region of the brachial plexus. The supraclavicular brachial plexus is seen at the center right of the image, just lateral and adjacent to the pulsating carotid artery with color flow. The first rib is seen just deep to the artery and plexus, providing a physical backstop to avoid inadvertent pneumothorax. An in-plane technique was used to advance the needle and anesthetic was deposited just superficial to the brachial plexus. The patient had improvement of his pain and was able to be discharged with outpatient orthopedic follow up.
Dr. Lindsay Howe, PGY3
Denver Health Residency in Emergency Medicine
Serratus Anterior Plane Block for PTX
20s M presented with acute onset atraumatic chest pain, and was found to have a large spontaneous pneumothorax on chest radiography. To augment pain control for chest tube placement, a serratus anterior plane block was placed using 20 mL of 0.5% bupivacaine and 20 mL of 1% lidocaine. The block is shown here, where the needle is seen in-plane instilling anesthetic in the plane between latissimus dorsi superficially and serratus anterior deeply. The anechoic pocket of anesthetic is seen to spread between the two muscles and dissipates quickly after injection is paused, indicating successful placement. This patient had adequate pain control and was able to have a pigtail chest tube placed and was admitted to the hospital.
Dr. Matthew Riscinti, Fellowship Director
Denver Health Ultrasound Fellowship
Supraclavicular Nerve Block
60s F presented with arm pain after a fall out of a wheelchair, and was found to have a proximal humerus fracture. A supraclavicular brachial plexus block was placed for analgesia. The brachial plexus is seen here, lateral to the pulsating subclavian artery, superficial to the first rib. The block is shown with the needle entering from the lateral aspect, depositing anesthetic adjacent to the brachial plexus just superficial to the first rib, which acts as a physical backstop, helping reduce the risk of inadvertent pneumothorax. Pleural slide is seen deep to the first rib lateral and medial , highlighting the proximity and underscoring the importance of keeping the entire needle in view during the entire nerve block procedure. This patient had improvement in their pain and was able to be discharged home.
Dr. Greg Wiener, PGY4
Denver Health Residency in Emergency Medicine
Supraclavicular Brachial Plexus Anatomy
Anatomy for a supraclavicular brachial plexus block.
Tom Jelic
@tomjelic
Lateral femoral cutaneous nerve block
Lateral femoral cutaneous nerve block. Clip attached is one of the actual block being performed for a male patient with a large vertical laceration along the lateral aspect of the proximal thigh.
Tom Jelic
@tomjelic
Fascia Iliaca Compartment Block
A 60s M presented with hip pain after a fall while skiing. He had a visible closed leg deformity but was neurovascularly intact. Radiographs confirmed a femoral neck fracture. A fascia iliaca compartment block was performed for analgesia and to facilitate orthopedic evaluation.
The first part of this clip shows the anatomy of the fascia iliaca, with the femoral artery (A), femoral vein (V), and femoral nerve (*) superficial and medial to the iliacus muscle (I). The fascia iliaca (^) overlies the iliacus muscle.
The later portion of the clip shows a fascia iliaca compartment block performed by inserting a needle from the lateral aspect until the tip is just deep to the fascia iliaca, and instilling a large amount (30-40cc) of anechoic local anesthetic in the fascial plane just superficial to the iliacus muscle (I).
The injection of anesthetic in this fascial plane allows the anesthetic to spread over a larger anatomic area, providing anesthesia to the lateral femoral cutaneous nerve and obturator nerve in addition to the femoral nerve.
Dr. Larry Benjey, PGY3
Denver Health Residency in Emergency Medicine
Interscalene Block
20s M with history of shoulder dislocations in the past presented with shoulder pain after boxing. He had a visible deformity to the shoulder, and radiographs confirmed an anterior glenohumeral dislocation. After documentation of a neurovascular exam, an interscalene nerve block was performed to facilitate reduction. The block is shown here, first with identification of the brachial plexus nerve roots (*) between the anterior and middle scalene muscles. The second part of the clip shows injection of anesthetic in the interscalene groove adjacent to the nerve roots. This patient had quick pain relief and closed reduction was achieved easily without sedation.
Tanner Muggli, PGY1
Denver Health Residency in Emergency Medicine

Median Nerve Dorsal Area of Anesthesia
Popliteal Sciatic Block
40s M presented with a laceration to the lateral lower leg after jumping through a window. To facilitate laceration irrigation and repair, a sciatic nerve block was performed at the popliteal fossa. The patient was placed in the contralateral decubitus position, and the linear probe was placed in the popliteal fossa in a transverse orientation to identify the sciatic nerve just proximal to the bifurcation into tibial and common peroneal nerves. This image shows the nerve block, with the needle entering from the lateral aspect, depositing anesthetic within Vloka’s sheath which surrounds the sciatic, tibial, and common peroneal nerves at the bifurcation. The block was performed just at the level of the bifurcation, and the tibial and common peroneal nerves are marked by the red asterisk (*) here. The patient had relief of pain, and the irrigation and laceration repair were able to be performed without any additional local anesthetic.
Dr. Rachel Vanderwel, PGY3, and Dr. Michael Heffler, PGY4
Denver Health Residency in Emergency Medicine

Common Peroneal Probe Location
Fascia Iliaca Nerve Block for GSW
Teenaged male presented with a single GSW to the medial thigh. The trauma evaluation revealed a displaced and shortened transverse femur fracture. To facilitate traction pin placement and provide analgesia, a fascia iliaca block was performed. The block is shown here, with the needle is seen entering from the lateral aspect and depositing local anesthetic just deep to the fascia iliaca (*), lateral to the pulsating femoral artery. The patient had improvement of his pain and was able to be admitted to the surgical floor for operative repair the next morning.
Dr. Phillip Breslow, PGY3
Denver Health Residency in Emergency Medicine
Posterior Tibial Block for Frostbite
60s M presented with foot/toe pain in the setting of recent freeze/thaw frostbite. To aid in analgesia, a posterior tibial nerve block was performed. The block is shown here, with the needle entering from the posterior/medial aspect, depositing local anesthetic adjacent to the tibial nerve (*). The patient had improvement of his pain and was subsequently able to be discharged.
Dr. Tyler Prince, PGY1
Denver Health Residency in Emergency Medicine
Dr. Nimish Bhatt, Fellow
Denver Health Ultrasound Fellowship
Supraclavicular Nerve Block for Elbow Dislocation
50s F presented to the ED from ortho clinic for recurrent elbow dislocation. She had previously been reduced 7 days prior and found to be re-dislocated in clinic. The patient required procedural sedation for her initial reduction. On this encounter a supraclavicular nerve block was performed using 20 cc of 0.25% bupivacaine with 15 cc injected deep to brachial plexus and 5 cc injected superficial. The block is shown here, with the brachial plexus (*) seen lateral to the subclavian artery (A). She tolerated the block well and had improvement in pain, but did ultimately require procedural sedation to facilitate reduction due to anxiety about moving the arm.
Dr. Fred Milgrim, PGY3
Mount Sinai Emergency Medicine Residency
Serratus Anterior Plane Block for Rib Fractures
50s M presented with side pain after a fall, and on imaging was found to have multiple unilateral rib fractures without other injuries. In order to help with pain control, a serratus anterior plane block was performed. The block is shown here, with the needle entering from the posterior/lateral aspect and placing anesthetic in the fascial plane (*) superficial to the serratus anterior muscle and deep to the latissimus dorsi muscle. This patient had improvement in his pain and was able to be discharged.
Dr. Riku Moriguchi, PGY3 and Dr. Smitha Bhaumik, PGY4
Denver Health Residency in Emergency Medicine
Interscalene Nerve Block for Shoulder Dislocation
20s M with history of recurrent shoulder dislocations presented with shoulder pain and deformity after being transferred from an urgent care after multiple unsuccessful attempts at reduction using intra-articular lidocaine alone. He was neurovascularly intact and clinically dislocated, which was confirmed on US. To facilitate reduction, an interscalene brachial plexus block was performed using US guidance. Shown here, the needle enters from the posterior aspect, approaching the brachial plexus (*) and depositing anesthetic adjacent to it. The patient had relief of his pain, and closed reduction was accomplished at the bedside without need for any additional analgesia or sedation.
Dr. Cheyenne Smith, PGY3
Denver Health Residency in Emergency Medicine
Erector Spinae Plane Block for Pancreatitis
30s M PMH chronic pancreatitis presented with epigastric pain, failing conservative management and continuing to have breakthrough pain on his home PO opiates. He was scheduled to have a celiac plexus neurolysis later in the month with interventional radiology but presented for uncontrolled pain. He had been given multiple doses of IV opioids in ED without effective pain control. An US guided erector spinae plane block was performed as shown. The needle is seen entering in-plane with a probe placed in the sagittal plane, and advanced until touching the transverse process (*), and injecting anesthetic within the fascial plane between the transverse process and the erector spinae muscles. The patient had effective control of pain and was able to be discharged home.
Dr. Nhu-Nguyen Le, Fellow
Denver Health Ultrasound Fellowship
Transversus Abdominis Plane Block
A transversus abdominis block is shown, with the needle approaching in plane, passing through the external oblique muscle superficially, then the internal oblique muscle in the middle, and depositing anesthetic in the fascial plane below the internal oblique muscle and superficial to the transversus abdominis muscle. This nerve block provides anesthesia of the hemi-abdomen and is useful in providing analgesia for conditions like appendicitis or diverticulitis.
Dr. Nhu-Nguyen Le, Fellow
Denver Health Ultrasound Fellowship
Erector Spinae Plane Block Approach
An erector spinae plane block is shown here, with the needle approaching in plane to touch the transverse process (*), and preparing to deposit anesthetic in the fascial plane between the transverse process and overlying erector spinae muscles. This block is generally best performed with the patient sitting facing away from the clinician, the US transducer in a parasagittal orientation just lateral to midline on the painful side, with an in plane approach, inserting the needle from the cranial or caudal aspect.
Dr. Nhu-Nguyen Le, Fellow
Denver Health Ultrasound Fellowship
PECS 1 Block
A PECS 1 block is shown here, with the needle entering from the superior and medial aspect, passing through the more superficial pectoralis major muscle and depositing anesthetic in the fascial plane between the more superficial pectoralis major and deeper pectoralis minor muscle. This nerve block provides analgesia to the anterior thoracic wall and is useful for breast or chest wall procedures such as I&D. The pleura is easily seen in this clip, which reinforces the importance of careful needle handling to avoid inadvertent pneumothorax or intrapleural infection.
Dr. Nhu-Nguyen Le, Fellow
Denver Health Ultrasound Fellowship
Popliteal Sciatic Nerve Block for Lac Repair
30s F presented with multiple self inflicted lacerations to the leg. To facilitate laceration repair without using a near toxic dose of lidocaine, a popliteal sciatic nerve block was performed. The block is shown here with the needle approaching from the lateral aspect of the popliteal fossa, in plane with the probe, depositing anesthetic next to the popliteal nerve (*). The anesthetic in this clip is outside of Vloka’s sheath, which encompasses the sciatic nerve and its more distal branches, the common peroneal and tibial nerves. Accordingly, onset of anesthesia in this patient was delayed, and so the laceration repair was completed using a combination of local infiltration of anesthetic as well as this nerve block.
Dr. Kathleen Joseph, PGY3
Denver Health Residency in Emergency Medicine
Median Nerve Block
30s M presented with a unintentional laceration to the middle finger nailbed while preparing food with a knife. To provide pain control and facilitate nailbed removal and repair, a median nerve block was performed. The block is shown here, first with a survey scan of the distal volar forearm showing the median nerve (*) deep to the flexor digitorum superficialis muscle bellies and superficial to the flexor digitorum profudus muscle bellies. The nerve was anesthetized using an in-plane approach, with the needle depositing anesthetic in the fascial plane adjacent to the median nerve. The patient had improvement in his pain. He ultimately declined nailbed repair but had good pain control and was discharged with outpatient orthopedic follow up.
Dr. Nimish Bhatt, Ultrasound Fellow
Denver Health Ultrasound Fellowship
Serratus Anterior Block
30s M presented with atraumatic acute onset chest pain in the context of inhaled marijuana use, and was found to have a spontaneous pneumothorax. The patient was hemodynamically stable, so a serratus anterior plane block was performed for analgesia and to facilitate pigtail chest tube placement. The block is shown here, with the fascial plane (*) between the serratus anterior muscle (deep) and latissmus dorsi (superficial). This block was performed using an out-of-plane approach, depositing anesthetic in to the fascial plane. This patient had mixed analgesic efficacy and so required additional anesthetic for chest tube placement, and was then admitted for further management.
Dr. Cody Brevik, PGY4, Denver Health Residency in Emergency Medicine
Dr. Nimish Bhatt, Fellow, Denver Health Ultrasound Fellowship
Erector Spinae Plane Block for Pancreatitis
30s M PMH ETOH pancreatitis presented with epigastric and upper abdominal pain in the setting of running out of his analgesic medications. To aid in pain control, an erector spinae plane block was performed. The block is shown here, with the needle entering from the cranial aspect to the thoracic process (*). Anesthetic was injected and observed to spread in the plane between the transverse process and the overlying erector spinae muscles. The patient had significant improvement in his pain and was able to be discharged with outpatient folllow up.
Dr. Nhu-Nguyen Le, Fellow
Denver Health Ultrasound Fellowship
Serratus Anterior Plane Block for Herpes Zoster
60s M presented with unilateral chest pain and a rash, and was ultimately diagnosed with a flare of herpes zoster. To aid in pain control, a serratus anterior plane block was performed. The block is shown here, with the needle advanced using in-plane guidance to the fascial plane (*) between the deeper intercostal muscles and more superficial serratus anterior muscle, where anesthetic was injected. The patient had improvement in their pain and was able to be discharged.
Dr. Henrik Galust, PGY4
Denver Health Residency in Emergency Medicine
Interscalene Brachial Plexus Block for Recurrent Shoulder Dislocation
30s M with PMH of many previous shoulder dislocations presented to the ED with pain and reduced ROM of shoulder after lifting his arm slightly. Radiographs confirmed an anterior shoulder dislocation, so an interscalene brachial plexus nerve block was performed to facilitate closed reduction without the need for procedural sedation. The block is shown here, with the needle entering from the posterior/lateral aspect with the tip adjacent to the brachial plexus (*), just posterior to the anterior scalene muscle which is seen at the left of the image. The block was effective, and the shoulder was reduced without need for additional medications.
Dr. Fred Milgrim, PGY3
Mount Sinai Emergency Medicine Residency
Fascia Iliaca Block for Intertrochanteric Femur Fracture
A teenaged male patient presented with hip pain and inability to ambulate after a fall off of an electric scooter. XRs demonstrated an intertrochanteric femur fracture, and CT ruled out other involvement of the pelvis or femoral head. To provide analgesia, a fascia iliaca block was performed. Shown here, the needle enters from the lateral aspect, lateral to the femoral nerve, artery, and vein which are seen at the top right of the image. Anesthetic is spread along the fascial plane shown (*). This patient had improved pain and was able to be admitted to the floor for surgery the next day.
Dr. Lee Johnson, PGY2
Denver Health Residency in Emergency Medicine
Fascia Iliaca Compartment Block for Hip Fracture
An elderly female presented with hip pain after an unwitnessed fall at her nursing home, and was found to have a shortened, rotated lower extremity, and after a broad workup was found to have a proximal femur fracture. To aid in pain control, a fascia iliaca block was performed under US guidance. The block is shown here, with the needle entering from the lateral aspect and injecting anesthetic in the fascia iliaca fascial plane. As seen by the very superficial femoral cortex, this 90s year old female was quite sarcopenic, so the normal muscular sonoanatomy is limited. The fascial spread seen in this clip helped to confirm appropriate placement of anesthetic. This patient was able to be admitted for surgery and had significant pain relief.
Dr. James Sutton, PGY3
Denver Health Residency in Emergency Medicine
Interscalene Brachial Plexus Block for Shoulder Dislocation
A 20s M with past medical history of prior shoulder dislocations presented with atraumatic shoulder pain and decreased range of motion after he felt a pop while playing sports and reaching across his body. He was found to have an anterior shoulder dislocation without fracture or neurovascular compromise. To facilitate reduction without procedural sedation, an interscalene brachial plexus block was performed. Shown here, the needle enters from the lateral/posterior aspect and the tip is placed adjacent to the brachial plexus, which is seen as 3 hypoechoic circles in a relatively vertical line deep to the sternocleidomastoid muscle. Anesthetic is injected sequentially lateral, deep, medial, and then superficial to the brachial plexus. This patient had relief of pain and his shoulder was able to be reduced at bedside without additional sedation or analgesia.
Dr. Larry Benjey, PGY3
Denver Health Residency in Emergency Medicine
Fascia Iliaca Block for Femoral Neck Fracture
A 90s year old female presented with hip pain after a fall off of a couch. Her workup confirmed an isolated femoral neck fracture in addition to acute metabolic encephalopathy and dementia. To provide analgesia while avoiding further sedation medications given her altered mental status, a fascia iliaca block was offered. After an informed consent conversation with the patient’s MDPOA, the block was performed as shown here. The needle is seen entering from the lateral aspect, injecting anesthetic along the fascia iliaca lateral to the femoral neurovascular bundle. This patient had improved pain and was able to be admitted for further management.
Dr. Cheyenne Smith, PGY3
Denver Health Residency in Emergency Medicine
Median Nerve Block for Carpal Tunnel Syndrome
60s F presented with intractable wrist pain due to known carpal tunnel syndrome. The patient was already established with hand specialist followup and had failed multiple other analgesics including a steroid course. To aid in analgesia, a median nerve block was performed. Shown here, the median nerve (*) is seen in the forearm, in the fascia plane between the flexor digitorum profunda and flexor digitorum superficialis muscle bellies. Anesthetic was injected in this fascial plane, adjacent to the median nerve. The patient had significant pain relief and was able to be discharged with hand specialist follow up.
Dr. Nimish Bhatt, Fellow
Denver Health Ultrasound Fellowship
Popping through the Fascia Iliaca
A 60s F presented with hip pain after a recent fall. Radiographs showed a subacute femoral neck fracture. To aid with pain control, a fascia iliaca compartment nerve block was performed. The needle is seen here popping through the fascia iliaca, just superficial to the iliacus muscle, before injecting anesthetic just below the fascia iliaca. This injection was somewhat intramuscular. The expansion of the anesthetic pocket with injection and collapse when injection is paused helps confirm that anesthetic is spreading along the fascial plane rather than pooling in a contained area within muscle.
Joseph Ponce, PGY-3
Denver Health Residency in Emergency Medicine
Erector Spinae Block for Nephrolithiasis
30s M with PMH nephrolithiasis in the past presented with acute onset flank pain. POCUS demonstrated mild hydronephrosis, and his workup was not suggestive of renal insufficiency or UTI, so aggressive symptom control was pursued. He was still experiencing significant pain after two doses of IV morphine, so an erector spinae plane block was offered. After informed consent and setup of supplies, the block was performed and is shown here. The transducer was placed in a sagittal orientation on the mid back at the level of T9, just lateral of midline (toward the affected side) in order to visualize the transverse process. A clip is shown here highlighting the transverse process, and the probe slides laterally to show the more superficial ribs with sliding pleura visible deep to them. The erector spinae muscle can be seen in long axis, just superficial to the transverse process. A 4 inch 20g nerve block needle was advanced using in-plane guidance until the needle tip contacted the transverse process, just deep to the erector spinae muscle. After a negative aspiration for blood, 30 mL of 0.5% bupivacaine with epinephrine plus 1 mL of dexamethasone (4mg in 1 mL) was injected deep to the erector spinae muscle. The patient had improvement of his pain and was able to be discharged with outpatient PCP follow up.
Dr. Michael Heffler, Fellow
Denver Health Ultrasound Fellowship
Median Nerve Block for Laceration Repair
30s M presented with a laceration to his thenar eminence. He was neurovascularly intact, and there was no concern for retained foreign body or fracture. To facilitate laceration repair, a median nerve block was performed. Shown here, the median nerve is seen in the fascial plane between the muscle bellies of the flexor digitorum superficialis and flexor digitorum profundus. A 27g needle was advanced using in-plane guidance into the fascial plane, and after a negative aspiration for blood, anesthetic was injected, with spread of anesthetic visualized surrounding the median nerve. The patient had significant improvement in his pain, and the laceration was able to be irrigated and repaired.
Dr. Michael Heffler, Fellow
Denver Health Ultrasound Fellowship
Popliteal Sciatic Nerve Block for Foreign Body Removal
30s M presented with a nailgun injury after he unintentionally fired a nailgun into his booted foot. To facilitate removal, a popliteal sciatic nerve block was performed. The block is shown here, where a 20g block needle was advanced using in-plane guidance until the needle tip was visualized adjacent to the sciatic nerve. Anesthetic spread was visualized within Vloka’s sheath, the nerve sheath which encompasses the sciatic nerve as well as its branches (common peroneal and tibial nerves). A total of 20cc of anesthetic was injected. The patient had complete resolution of his pain shortly thereafter, and the nail was able to be removed without difficulty.
Dr. Brigit Noon, PGY3
Denver Health Residency in Emergency Medicine
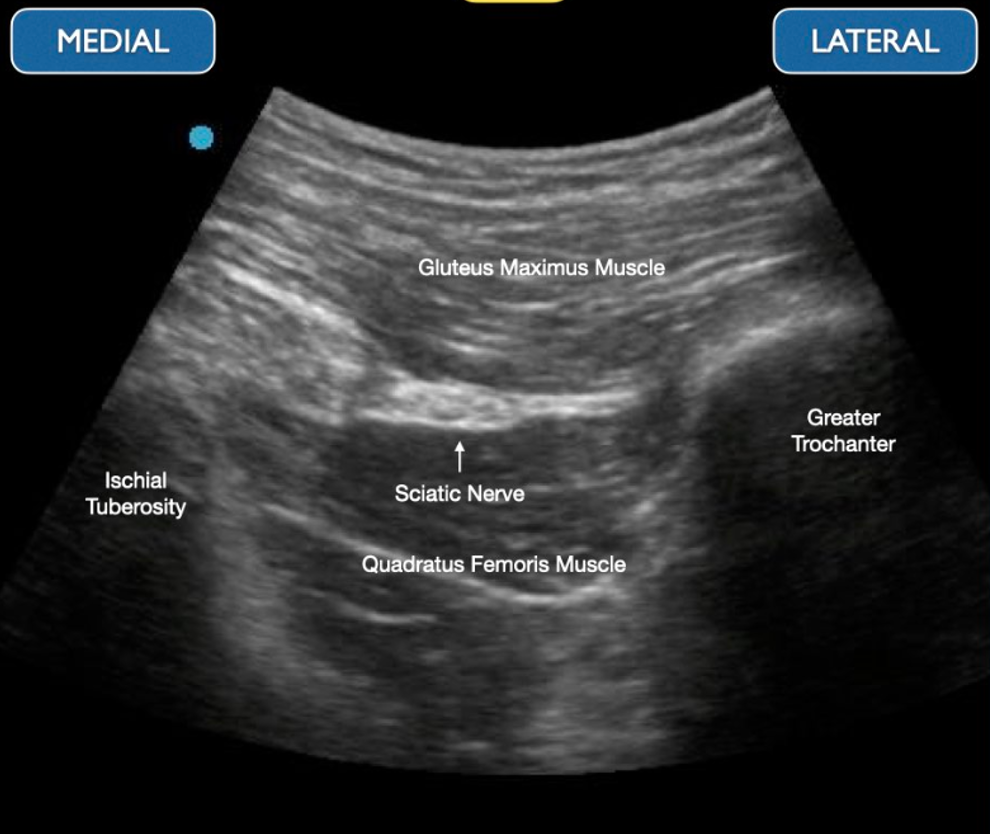
Transgluteal Sciatic Nerve Block Anatomy
Transgluteal Sciatic Nerve Block Anatomy 2

Transgluteal Sciatic Area of Anesthesia
Transgluteal Sciatic Nerve Block 1
Transgluteal Sciatic Nerve Block 2
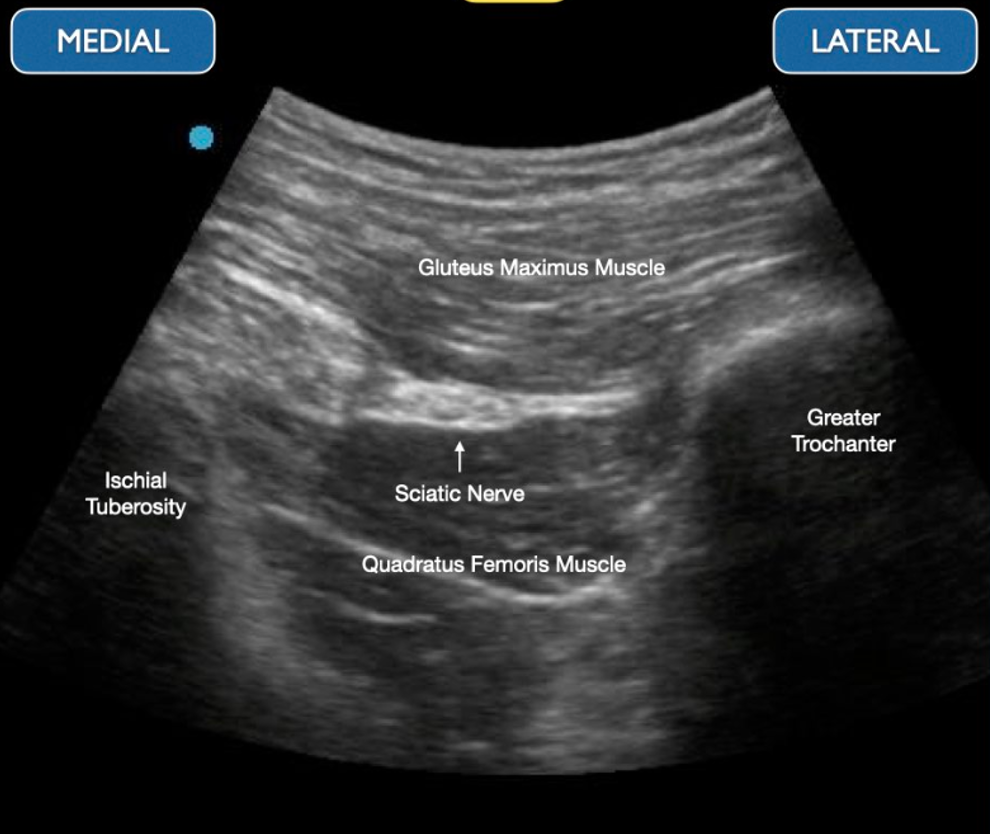
Transgluteal Sciatic Anatomy

Fascia Iliaca Nerve Block Hydrodissection
A 70s M w ground level fall pw a left femoral neck fracture. The needle can be seen approaching from the right of the screen (laterally) using an in-plane anteromedial approach. The pulsating left femoral artery is seen on the left of the screen (medial). Adequate hydrodissection is shown with 10cc of normal saline in the fascial space prior to depositing the anesthetic, 30cc of 0.2% ropivacaine. 45 minutes after administration, pain was significantly decreased and the patient was admitted for surgery.
Dr. Brigit Noon, PGY-4, Denver Health Emergency Medicine Residency
Dr. Matthew Riscinti, Ultrasound Fellowship Director, Denver Health Emergency Medicine
Erick Otiniano, MS4, University of California Riverside School of Medicine
Infraclavicular Brachial Plexus Nerve Block
A 71-year-old male presented to the ED one day after a ground level mechanical fall during which he sustained a L shoulder injury. Given his age and initial borderline blood pressures, he received CT images of his chest, abdomen and pelvis which initially revealed a minimally displaced humeral head fracture extending into the greater tuberosity. His workup was ultimately otherwise unremarkable. He was consented for an infraclavicular block for pain control prior to being placed in a cuff and collar sling.
The needle can be seen approaching the axillary artery, around which the lateral, posterior and medial cords of the brachial plexus lie anatomically. The needle approach is from cephalad to caudal, with the ultrasound probe placed in the deltopectoral groove. The goal of this block is to deposit anesthetic at the 6 o’clock position relative to the axillary artery. Anesthetic can be seen depositing just superior to the axillary artery, around the 7 o’clock position (screen right). A total of 20 cc of 0.25% bupivicaine with 4 mg of dexamethasone was used.
Prior to the block, the patient’s pain score was an 8 out of 10, with significant pain with passive or active range of motion. Shortly after the block, his pain decreased to a 2 and he started ranging his shoulder with minimal discomfort. He was placed in a sling and ultimately stayed in the observation unit for frequent falls and PT/OT evaluation.
Dr. Spencer Seballos, PGY-2, Denver Health Emergency Medicine Residency
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
Adductor Canal (Saphenous) Nerve Block
A 58-year-old woman presented to the ED two weeks after being bitten on her right thigh by her dog with a growing abscess over the medial thigh just superior to the knee. In order to facilitate abscess drainage, a combination of femoral nerve and adductor canal (saphenous) nerve blocks were performed. Seen here is the saphenous block. The transducer was placed over the middle third of the thigh on the medial aspect. The needle is seen approaching from lateral to medial with the femoral artery pulsating at the bottom of screen right. The adductor canal contains the saphenous nerve, the femoral artery and femoral vein. It lies just deep to the sartorius muscle, lateral to the vastus medialis and medial to the adductor longus muscle. 10 cc of 1% lidocaine without epinephrine can be seen hydrodissecting the fascial plane just deep to the sartorius muscle. The patient then underwent a pain free abscess drainage.
Dr. Wesley Ng, Ultrasound Fellow, Denver Health Family Medicine
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
Dr. Matthew Riscinti, Ultrasound Fellowship Director, Denver Health Emergency Medicine
Erector Spinae Nerve Block
A 43-year-old female presented to the ED with four weeks of ongoing R sided costovertebral angle and anterior chest wall discomfort, previously having been treated for pyelonephritis at the onset of her pain. Given her nonspecific symptoms that had been refractory to standard management, a right sided erector spinae block was offered for analgesia. The needle can be seen approaching the T6 transverse process (the approximate site of her pain) from cephalad. The erector spinae muscle is lifted off the transverse process with good spread in the fascial plane demonstrated in the subsequent images. 30 cc of 0.33% bupivacaine with 10 mg of dexamethasone was used. The patient had moderate pain relief.
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
Ulnar Nerve Block
A 45-year-old male presented to the ED with an accidental self inflicted laceration to the hypothenar eminence of his R hand sustained from a pocket knife. He received an ulnar nerve block for pain control. The ulnar nerve can be seen separating from the ulnar artery as the probe is fanned up the medial aspect of the forearm. The needle can then be seen approaching the nerve from medial to lateral and approximately 5 cc of 2% lidocaine was deposited just lateral to the nerve. The patient then underwent a pain free laceration repair.
Danielle Bobzien, PA, Denver Health Emergency Department
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
Erector Spinae Block for a Traumatic Injury
A 45-year-old male presented to the ED as a pedestrian struck by a car. He was hit from behind and pinned to a wall briefly. Workup revealed left sided 1st-5th anterior rib fractures, 3rd-7th posterior rib fractures with significant displacement, as well as left C7 and T1 transverse process fractures and a left medial clavicle fracture. An erector spinae block was performed for analgesia. In the first image, the erector spinae muscle layer can be seen sitting atop two levels of transverse processes. The patient was slowly rolled onto the right lateral decubitus. The second clip shows a needle approaching from cephalad and depositing anesthetic into the fascial plane between the erector spinae and transverse process. The patient felt near immediate pain relief at the termination of the procedure. He was subsequently brought to the SICU prior to having a rib plating operation the following day, and received a serratus anterior catheter placed by anesthesia during pre-op.
Dr. Makenna Rice, PGY-1, Denver Health Emergency Medicine Residency
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
Transgluteal (Proximal) Sciatic Nerve Block
A 36-year-old male presented to the ED with acute onset left sided back pain that started suddenly 6 hours prior to arrival while bending over. The pain radiated down his left leg and he had a positive straight leg raise with a severely antalgic gait. A transgluteal sciatic nerve block was performed. The patient was positioned in the right lateral decubitus position with the left hip and knee flexed. The needle can be seen approaching from lateral to medial, just over the greater trochanter. The needle reaches the fascial plane between the gluteus maximus and quadratus femoris muscles where the sciatic nerve and inferior gluteal artery lie. The plane is seen separating with hydrodissection using 20 cc of 0.5% bupivacaine with 10 mg of dexamethasone. The patient had complete relief after the block and was able to ambulate out of the department with ease.
Dr. Kate Simeon, PGY-4, Denver Health Emergency Medicine Residency
Dr. Fred Milgrim, Ultrasound Fellow, Denver Health Emergency Medicine
PENG Block
A PENG block was performed using the linear probe. The hyperechoic psoas tendon can be seen lifting off the ileum with the injection of anesthetic.
Ariella Cohen MD
Eric Quinn MD
Maimonides Medical Center Emergency Medicine